When to Suspect MCAD

The acronym MCD is the (new in 2022) umbrella term for ALL forms of Mast Cell Diseases or Disorders, including the very rare (thankfully) MC Leukemias, followed by the still rare but less so forms of Mastocytosis (several, including cutaneous and systemic); and lastly the newly but most poorly recognized yet quite common form of Mast Cell Activation Diseases (MCAD) now called Mast Cell Activation Syndrome or MCAS for which an ICD-10 code finally came out in October 2016.
Editor’s note 9/17/23: I’m just now starting to re-write this entire site to reflect the new umbrella term MCD to represent the entire collection of Mast Cell Diseases, which includes all forms of Mastocytosis, plus all forms of MCAD (MCAS, HaTS, MMAS, and anything else we uncover that involves inappropriate mast cell over-activation.) Please forgive any outdated or erroneous leftover writing. We used to use MCAD as the umbrella term. (Still trying to catch up, April 2024.)
2016: Oh, and let’s not forget the new dx on the block, Hereditary Alpha Tryptasemia! Aka HaTS. (I was in the study that helped uncover it in 2012.) It is suspected in folks with elevated baseline tryptase levels within their families and signs of Hypermobility Spectrum Disorders/hEDS and IBS.
MCAS may run as high as 10% of the population we are now realizing. I’ve seen some sources cite as high as 14% and even higher in one case. Not rare at all! Just rarely recognized. Find best articles for your doctors to learn more here on my MCAD resources page.
All forms of MCDs, but especially MCADs cause what you might call “extra” allergies & sensitivities in the absence of elevated IgE for same that your allergist can’t easily test for due to the the lack of IgE antibodies driving it. You may have plenty of “regular” IgE-driven allergies also, but those can be diagnosed more easily and only involve organic proteins. (Pollen, dander, bugs, foods.)
Yet we suffer from over-activation of our mast or “allergy” cells which are throughout your body but especially the skin and GI tract. (I secretly wish we’d rename it “MCOAS” for Mast Cell OVER-Activation Syndrome, but that’s just me.)
It also runs in all races and ethnicities and skin types. (I’m slowly updating the below to better reflect this in 2022. Most literature only refers to the appearance in white skin yet, sorry.)
Folks with Mastocytosis have too many and/or misshapen mast cells in clumps in various places throughout the body (on the skin, and/or in the bone marrow or GI tract) which may or may not also be over-active. They may have to treat for both (over) activation and proliferation. But some just treat or monitor their proliferation.
Folks with MCAS and HaTS have normal or lower numbers of mast cells more evenly distributed (not clumped together usually, and normally shaped) but they are highly reactive and too easily triggered making them very sick still.
MCAS is not necessarily less severe than masto either – some patients with “just” MCAS can be more anaphylactoid than some masto patients. It really varies.
You can be just as reactive and go into anaphylaxis from any form of MCAD as from “traditional” *(IgE-driven) allergies and (IgG) sensitivities, but also to non-protein substances including chemicals like chlorine and fluoride, scents, hormones, exercise, temperature changes, pain, stress, sunlight and vibration to name a few. Yes, crazy making and challenging to live with!
And partly why the MCA diseases are so hard to recognize – they drive and/or mimic many other diseases and conditions, much like a chameleon. They’re hard to differentiate and properly diagnose for everybody.
Many people accidentally use the term MCAD to mean MCAS only, and many use the two terms interchangeably. (It doesn’t help they are off by only one letter on English keyboards either.) While technically incorrect, in the end, it’s the inappropriate mast cell over-activation in all cases that is aggravating us and sending us to the doctor (no matter how many mast cells we have and in what shape) so I don’t get too worked up about it. Just be sure to rule out mastocytosis and leukemia when appropriate. And do not use mastocytosis as the umbrella term any more.
(I was pleased to see the Mastocytosis Society actually change their name to The Mast Cell Disease Society for this very reason in 2020, thank you!)
Anaphylaxis comes in grades by the way, though doctors and EMTs are usually only interested or concerned with the highest levels/throat closing signs since that’s when it can kill you, and is what your school nurses are constantly watching for. Knowing the milder signs/levels can help you stay calm and medicate in time (or get away from a trigger) to help avoid it escalating to that level. (Staying calm really helps.)
No two people will have the same course of symptoms when reacting either. Some also react slower than others – we call ourselves “lucky leakers”, vs shockers. Finding this info useful? I can really use your support at any level here, TY!
So When to Suspect It?
This is accordingly really tricky, as truly no two patients even with the same form will present alike, even in the same family. As we say about some other conditions, it’s truly as individual as fingerprints just like EDS. Thus it is extremely widely varying in nature of onset, course, and response to medications as the brilliant US hematologist Dr. Lawrence Afrin depicts so thoroughly in his new book Never Bet Against Occam (Amazon 2016). (Highly recommended for both patients and doctors to read – both will find it validating in different ways.)
However, there are some common “themes” and experiences I am listing here, noting that this list is by no means official, nor comprehensive, no two patients will experience all of these issues, but most will experience a good handful if I’m on the right track. (This list is not officially endorsed by anyone yet.) Again, use this as a starting point for suspecting a form of MCAD with your doctor.
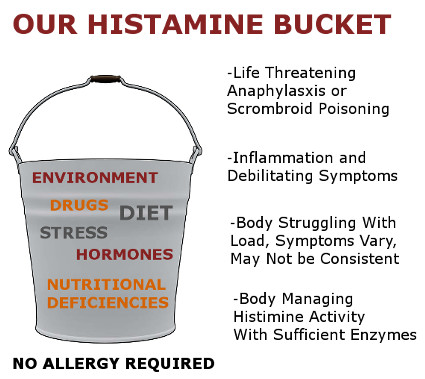
And yes, it highly resembles Histamine Intolerance, which is a flip-side of the same coin: failure to out-process (metabolize and degrade) histamine leading to the signs of excess, vs over-production of histamine from over-activation.
And yes, some poor souls may even have both, along with methylation issues lending to even higher histamine levels in the body. (Try to keep your histamine levels down, both by not adding any from high histamine foods, avoiding triggers – so you don’t produce your own, and making sure you out-process what you do have okay.)
I’m increasingly convinced MCAD-driven inflammation probably underlies a large percentage of ER cases that are diagnosed as “just anxiety” or panic attacks, or angina and heart attacks that show no signs of heart disease. (Do play it safe and get yourself checked out if suspect any heart problem!) Hopefully this list will help folks to know when to suspect it:
- Easy flushing darker or red, particularly of the “mantle” (upper chest, neck and face, not always 100%), and especially to stress, heat or triggers (including emotional)
- Hives, especially stress-driven ones, can be large or small and not always all over
- Urticaria Pigmentosa (persistent hives or bumpy “freckles” that fade but never disappear, and itch during reactions), TMEP, Purpura
- Dermatographism – aka “skin writing” where you either turn dark or red easily or even get a hive-like welt (wheal) with a light skin scratch. (Google it for images.) You may notice (darker or red) indented sock & underwear “tattoos” where the elastic rests on your skin in winter
- Adult onset or flare-ups of acne
- Sudden onset diarrhea especially alternating with constipation (often called IBS)
- Sudden abdominal bloating and swelling (can look “pregnant” when you’re not)
- Sudden onset of gas and belching
- Sudden onset nausea, trouble swallowing (rule out comorbid HDCT driven neurological drivers of this), early satiety
- Tendency to run cold (but can alternate with sudden hot flashes/sweating bouts or run hot also)
- React easily (are sensitive) to sunlight, vibration, startling, pressure, stress, hot or cold
- Sensitive to alcohol and molds (the penicillin class of anti-biotics, mushrooms)
- Reaction to bee stings and iodine contrast dyes, local & general anesthesia
- Itching of unknown origin, may migrate, often severe
- Tingling or burning sensation anywhere in the mouth or GI tract (BMS)
- GERD
- Tinnitus of all kinds, but especially after eating certain things
- Variable blood pressure (BP), may run quite high or low on average and can swing widely at times. Some have a spike with anaphylactic reactions, followed by later drop.
- Angio-edema (swelling) especially that “migrates”, e.g., shows up in different places (lips, eyes, hands, feet), not always in the same place nor due to being upright (gravity-driven)
- Shortness of breath and asthma like symptoms and outright asthma
- Hair loss/thinning
- A persistent non-productive but wet-sounding cough with no identifiable infectious origin
- Chronic post-nasal drip or rhinitis in the absence of allergies
- Watery eyes, burning eyes (feeling of granularity or sandiness behind eyelids)
- Rashes of unknown origin, adult onset acne or acne-like spots (not same as Urticaria Pigmentosa which is a form of cutaneous mastocytosis)
- Easy nose-bleeds (epistaxis) of unknown origin, easy bruising or bleeding (w or w/o a comorbid connective tissue disorder)
- Slow wound healing
- Aquagenic urticaria (your skin reacts to immersion in water)
- Sudden weight gain or loss in absence of clear driver/cause (rule out lipedema and endocrine disorders)
- Sudden mood swings, anger bouts or irritability (we call this the “histameanies” in support circles, smile, and thank everyone for tolerating us through them)
- Cry easily, easily aroused, emotional (look into histadelia)
- Sudden anxiety or panic attacks followed or accompanied by additional signs of low-level anaphylaxis (skin signs, mucus, etc.)
- Sudden onset aphasia, or loss of words or speech, slurred speech or “word salad” and confusion that clears up after the reaction/stress subsides or with anti-histamines or mc stabilizers (be sure to rule out stroke! as well as epilepsy).
- Any and all forms and levels of anaphylaxis which comes in grades. It’s also different/harder to quantify under anesthesia as noted here.) Many are in mild constant low level state with occasional spikes to higher states or rebound events. (Most medical personnel refuse to call it anaphylaxis until it’s the higher level/s however be prepared for some differences of opinion here and try to stay calm and keep your epi and Benadryl handy.)
- Sensitivities or anaphylaxis to any and all drugs, fillers, dyes, additives, preservatives, fluoride, chlorine, etc. We can react to any degree to almost anything, truly. (Yes, crazy making for all.) Sometimes it’s not the active ingredient, but a dye or filler. Or the fact you were upset when you ingested it.
- Esophageal spasms, nutcracker esophagus, especially when stressed
- Chronic fatigue, sometimes severe, often identical in onset/nature to opioid-induced respiratory depression (many find this in reaction to gluten and dairy) often misdiagnosed with Chronic Fatigue Syndrome
- Pre-syncope – or dizziness, light-headedness, feeling about to faint (but you don’t)
- Full syncope – full fainting (less common but also happens)
- Clotting or alternatively bleeding disorders (either direction) that defy normal hematological diagnosis and workup (and treatment)
- Swollen lymph nodes of unknown origin, not true lymphomas
- Any other forms of hematologic disorders (strange cell counts/sizes, changes in same) that do not strictly match true workup for similar conditions (e.g. polycythemia in absence of the JAK2 mutation) or don’t respond appropriately to treatment for same
- Migraines and cluster headaches, hydrocephalus and “corking” driven dysautonomia
- Low blood volume from 3rd spacing and urinating more than ingesting during reactions (lends to BP drops and very low BP)
- Kounis Syndrome or signs of it. (Allergy-type driven MI/vessel spasms)
- Interstitial Cystitis (IC) or chronic UTI’s that don’t resolve easily or at all with anti-biotics (i.e. “sterile” inflammation)
- Women may notice “flares” of these symptoms on a monthly basis from their cycles, and or during lifetime hormonal changes, especially any time after age 30 from peri-menopause
Addressing MCAD
Again, this list is neither official, nor comprehensive, but is a start for when to suspect these very tricky to diagnose Mast Cell Activation Diseases.
A very large dose of patience is in order – very few doctors are up on the the prevalence of the conditions yet even in May 2016 – nor know how to diagnose (very tricky, no single easy test for all) and how to treat (equally tricky: no single easy medication course works for all, and you may react to any and everything including known helpful medications for others – always start low and slow until you know).
Generally avoiding stress and high histamine foods (leftovers, ground meats, fish) and taking anti-histamines seems to be helpful on the whole.
Please be very patient, try to log and track triggers for yourself (and then avoid them as able), be mindful of your mood, condition and environment (including temperature and scents) at all times (I can eat chicken when calm but not when stressed or rushed, e.g.).
Try to eat single ingredients and whole foods vs complex or processed meals to reduce potential triggers and maintain best nutrition. (Some will fare better than others, some even react just to the physical act of eating, laughing, sex, travel etc. – yes, crazy-making as previously stated!)
Common comorbidities include heritable connective tissue diseases (especially some forms of Ehlers-Danlos Syndrome, notably the more common hypermobile type or a Hypermobility Spectrum Disorder), Fibromyalgia (often misdiagnosed hEDS or HSD in milder form), migraine, high cholesterol (increasingly recognized as a a sign of inflammation and not dietary driven), diabetes, auto-immune diseases of all kinds, CVID and all forms of primary immunodeficiencies (tendency to get sick easily and often), UTI’s, IC, easy bleeding (in absence of von Willebrands) and bruising, APABS (anti-phospholipid anti-body syndrome) and much more.
I’d like to suggest the chameleon as our official mascot: I’m starting to appreciate just how many diseases MCAD both mimics, and drives while going unrecognized for what it truly is.
I will add to this list as able. Again, it’s not meant to be comprehensive nor official yet, just suggestive. Consult a savvy* allergist to start, followed by a hematologist who is aware of MCAS as well as Mastocytosis if needed later. (*Not all allergists are aware of – nor believe in – MCAS yet, alas. You might join TMS to find a local support group to help you find the best doctors near you.)
See my MCAD Resources page for help with educating yourself and your doctors on the matter and consider joining The Mast Cell Diseases Society (now free!) for additional information and support for all forms of MCAD on and off line. Good luck! Last updated August 2022.


This is a very interesting read, I wish it talked more about treatment options
Thanks. I suppose I could add some at some point yes sorry. The main approaches involve identifying and avoiding triggers, including foods, meds, scents, environmental (e.g. temp, vibration) or lifestyle (high stress, trauma). And the use of anti-histamines (H1 and H2 blockers) and various mast cell stabilizers as appropriate. Quercetin is a known natural mast cell stabilizer you can get over the counter, but the powdered form is not as effective as a liposomed version such as Neuroprotek. (Google it.)
Some patients end up on cromoly sodium which is hard to get, may need to be special ordered and may not be covered by your insurance. (Policies vary, check.) And also ketotifen among some other meds. (Leukotrienes, inhalers, etc.) I highly recommend seeing an allergist /immunologist to start, then work your way up to a hematologist /oncologist as needed. (The latter may prescribe meds to counter mc proliferation when warranted for forms of mastocytosis.)
The problem is, we’re so darn sensitive and metabolize so differently, that no two patients will experience same course of treatment, and it’s all trial and error. Sometimes you may react to a med, but it’s really just the filler in a tablet you’re reacting to, not the active ingredient itself. Many patients find compounding their meds to work better in that case. Again, you can only learn through trial and error sorry.
Find support here: http://tmsforacure.org
HTH – Jan
Finding a doctor with MSAD knowledge is difficult. I live in NE Georgia .
I trust you’re referring to the state of Georgia in the US, not the country. Regardless, you might try finding a local support group under the TMS here – they can help you find any local doctors who might help you get diagnosed:
https://tmsforacure.org/
Also, please don’t be discouraged/take it personally. It is one of the single hardest conditions to get diagnosed, even in the sickest patients, unfortunately! I’m sorry this is so.
I was diagnosed by Dr. Hunt in Athens, GA. Don’t know if he is best for treatment, though.
Good to know, thanks Carolyn!
You mention sensitivity to “vibration”, are you able to expand on just what you mean by that term, and give some examples? Thank you!
Yes. Many of us find the vibration from car and plane engines to make us get suddenly drowsy/pass out if not fully react. I passed out on a short hopper flight that used a prop jet back east last time I tried one. (I’m better on the bigger planes so far.) I struggle to drive very far at all and take many safety breaks.
One fellow patient told me she can’t ride on the back of her boyfriend’s motorcycle – she literally passes out and falls off, yikes!
I did find that it’s worse whenever I’ve taken an opioid, but it still happens to some degree even when I have none in my system for over a week. HTH.
This is me!!! I can rarely drive for more than 20 minutes without getting very drowsy. Thankfully I rarely have to drive that far and when I do I almost always have a friend or my fiancé who can drive me to the place.
It’s nice to know you’re not alone nor crazy huh? We’ve found “our people” 😉
OMG! For YEARS, whenever I drive and particularly when there’s traffic (i.e. the car is “idling” and the vibrations are more noticeable), I get flushed and have to rush to a bathroom! I thought it was just the car “jiggling” my insides and making everything have to move! Glad to know this is a thing and I’m not just wacky. I actually had to buy a particular type of car that had VERY low vibrations, and now that it’s getting older, it’s vibrating more and making me want a newer one. Hmmm…. thank you!
So glad you found “your people”, and know you’re not losing your mind – just your body – or at least a mast cell granule or two! Welcome to the “pool”. Cheers,
Jan
My daughter and I think the Siamese Cat should be the mascot – because the Siamese Cat are very knowingly patient – They seemingly know more than their owners, patiently wait for their owners to figure things out, and they are mysterious. And as patients of this illness, we seemingly know more about ourselves than our doctors, the researchers, and the people around us – like friends and family, patiently wait for them all to finally understand us and give us what we need, and this illness is quite mysterious. Certainly, the Siamese Cat is mysterious, and this illness is mysterious. (and little children afraid of chameleons!) We could just sum it up in that one word – Mysterious! Xx
Ha! I like that – yes, we are mysterious – and quite patient – indeed!
I have been diagnosed with TMEP but also have symptoms of systemic mastocytosis as well. I am seeing an allergist tomorrow. Fairly certain that there will be a skin prick test done will it show any allergies caused by masto? Seems like all I have read online suggest that the testing wouldn’t be useful in cases of mastocytosis. I am so lost and it seems my primary care doc has no clue what to do with me.
So a little clarification is in order: Masto itself doesn’t cause “true” allergies which are IgE-mediated reactions. But it can lend to their being heightened in those who have allergies. And… you may find you react to some things >even in the absence of a IgE< lending to the confusion. I'm now convinced my underlying MCAS lent to my increased reactions to the skin prick tests of my youth. (My arms/back would swell up quite huge very quickly, causing them to wipe the serum off!) This comes from having a heightened histamine level over all in our bodies, making us sort of "hair-trigger" ready to react to almost anything. Some people have absolutely zero "true" allergies, that is, zero IgE-mediated reactions, yet are still very sick as though they had "allergies" because of either MCAS or Masto that hasn't yet been recognized. (Yes, TMEP is a form of cutaneous Masto I believe or a sign of at least a form of MCAD.) You may also have some true IgE-mediated "allergies" >in addition< to any underlying masto or MCAS. This just lends to your overall sickness level and reactivity. Does that make sense I hope? All forms of MCAD are rarely recognized, and some not at all yet, so this is often tricky to get allergists to see. HTH!
You are my long lost twin! Haha I’m kidding, of course…but I have spent my whole life thinking I am the only person who is really like this. Though I would not wish it on anyone else, it’s exciting to know I’m not alone. You do sound just like me. You describe the symptoms fairly similarly to what I’ve always tried to tell people. Thanks for sharing!
Lol – hi twin! And not surprised. 😉 You’re quite welcome, glad you found me. I’m semi-convinced we’re all part of one giant “Clan Dumpty” of Humpty fame, right? 😉
I am a nurse who has not been able to work due to severe anaphylaxis. I have had 9 reactions since August. Mostly to fumes and some unknown. Allergist is at his wits end. So I started researching myself. I have Celiac Disease and Adult Stills Disease. For many years I have suffered from severe arthritis, fatigue, unknown weight gain, salmon colored rashes (thought to be from the Stills), chronic diarrhea, GERD, edema, cold alternating with severe hot flashes, burning in GI tract, very sensitive to anything that touches my skin, the feeling of sand in my eyes, wet cough (smokers cough but I don’t smoke), asthma, dizziness, etc. My rheumatologist says that often there are many other diseases associated with autoimmune. I hardly leave my house because I react to everything. I found this site and plan on calling my rheumatologist tomorrow.
I’m so sorry for your health challenges, but glad I might be helping you close in on a likely answer. That is a classic story of the path to an MCAD diagnosis – many are diagnosed with “idiopathic anaphylaxis” as the allergists fail to find IgE drivers. We’re finding SO many other ways to trigger mast cells and basophils besides proteins that generate IgE antibodies alas including chemicals (chlorine, fluoride), scents, vibration, stress, pressure and temperature (hot or cold). Definitely check out my resources page for more to help with your diagnostic journey, and settle in – it’s a marathon I’m afraid due to the lack of awareness and updated info in the medical world yet:
http://ohtwist.com/what-is-mcad/mcad-resources/
Good luck!
I just saw that you mentioned Basophils, I have gone to the hospital many a time with panic attacks and blood pressure spikes, heart arrhythmia and one thing they’ve told me consistently is that my Basophils are always low. Does mast cell cause low Basophils or high? And thanks for the info about MCAD, I’m beginning to look into this to explain my own health issues: Choking and mucus feeling nearly all day everyday, low and high BP, arrhythmia, rashes, a bright red face and swelling, migraines, IBS, GERD, weight gain, fibromyalgia.
I don’t recall mentioning basophils (and a quick search doesn’t show any mention on this particular page of mine) but… I vaguely recall Dr. Diana Driscoll of PrettyIll.com mentioning them as a potential contributor to MCAS. Like, maybe they get the part started? That said, it’s merely a total hypothesis (WAG) on her part, not based on any research to my knowledge.
I had to pause and check before answering this too, as I first confused them with eosinophils, which we do seem to attract more of. (They are attracted to mast cells by chemo-taxis apparently – like ants following ant trails right?) I do see a statistically significant amount of Eosinophilic Esophagitis (EoE) in the community. But different cell, I know.
Great question. And… regardless, you’re describing lots of symptoms of MCAS for what it’s worth. HTH.
After an anaphylactic reaction due to an unknown food, I finally had allergy testing today and it showed I was only allergic to venom (I’d had an episode due to yellow jackets once a couple of years ago). However, I had an outrageous reaction to the positive control histamine. For the intradermal test, the spot on my arm looked like a quarter with the thickness of a nickel was trying to push its way out of my arm and the lab tech/nurse said the redness was unmeasurable, and would have to be noted as the maximum of 45 rather than the three or so inches it truly was. I asked a lot of questions and she said I basically was allergic to myself by being allergic to the chemical histamine that your body produces. Basically, we’d found our answer, she said. When I mentioned it appeared I was allergic to histamine to the doctor, she said everyone is supposed to react to the histamine. And that was that.
She had me have blood work done, and I am supposed to go back in two weeks. Should I call her and further explain what happened in the lab? I feel like I came home so empty handed. She did say she expects the blood work to show nothing and suspects mast cell issues, though she seems more mystified, where the lab tech/nurse, though she probably shouldn’t have, felt confident in diagnosing me.
Boy that’s a toughie – and an all too common experience I’m afraid, where an allergist is afraid to go out on a limb and recognize a form of MCAD, but a nurse or tech isn’t. I would try bringing her some info, especially this article from Dr. Afrin (if not his actual book) to help her along:
https://www.novapublishers.com/catalog/product_info.php?products_id=42603
Which is on my MCAD resources page from which you can harvest all you like here (nay, I recommend it):
http://ohtwist.com/what-is-mcad/mcad-resources/
At a minimum, it sounds like you have a high baseline histamine load to get such a large wheal (raised patch at the test scratch site) like that. (Aka “dermatographism” – google it.) I would at least suspect you of a form of MCAD at a minimum. The $64B Q is can you get it diagnosed – even some of the sickest patients struggle to get positive test results, so in the end, as long as a doctor will help treat you presumptively and recognize your symptoms and suffering, you’re just as well off in some ways.
If she (the doctor I presume) will not, you may need to try to find another. I’d seek support from these guys in the process:
http://tmsforacure.org
Hope that helps, good luck!
My daughter has had issues with what finally got diagnosed as “abdominal migraines” for several years now. She is 16. She has frequent nausea and will commonly awaken vomiting repeatedly for a few hours then exhaustion. Her maternal grandmother had EDS as well as her mother (me). Could this be MCAS?
I’ve been wondering this myself for a while. I don’t get what people call “migraines”, so have not paid close attention to the definition of them, but I had wondered when I heard people describing “abdominal mingraines” if that might not be the case.
I’m not a doctor, but my intuition says I think it could well be mast cell driven. And, one way to figure it out would be a) to not only try to find her triggers (food, scent, chemical etc.) , but also b) treat for MCAS (antihistamines and quercetin are over the counter, with y our doctors okay) and see if it helps. (If you’re not already.)
They sure sound like (mild or more) pre-anaphylaxis to me… (nausea, vomiting).
Hi
Histamine can build up heavily in tissues if your b vitamins are deficient. To make sure it’s not just histamine overload take high B6 with your food. And to slowly dissolve the accumulated one take niacin, or B3. But to avoid very severe reactions take tiny amounts of B3 slowly. You will flush. This is good. This is what you want. This action vasodilators and dissolves histamine. After a week or two of this do the arm prick again. This time you may get a very different response. As an aside, you may need lots of methylfolate too. Follow your reactions…Good luck.
Great insight into yes, yet another onion layer to peel back, so to speak. There are multiple factors that can lend to why some are higher histamine (histadelic) than others, not all due to MCAS. Thanks for the insight. (I so wish doctors had good nutritional training, sigh.)
And again, work with your doctors everyone – over methylating can cause trouble too. 😉
I was diagnosed with Dermatographia last year. Reading this after it was posted in a group I am in I have multiple of these symptoms. I am going to mention this to my doctor as I have a appointment in two days.
Glad I could help you to suspect the condition. Don’t be surprised if they haven’t heard of it, it’s poorly known in the medical community yet, but do harvest some of the top literature for doctors here on my resources page to that end:
http://ohtwist.com/what-is-mcad/mcad-resources
Good luck!
My name is Corrie and I’m. 48yr old mother of 2 children. I just had an appointment with an immunologist here in the UK (Glasgow to be specific)
I found the consultation really difficult. I left not knowing what the consultant was testing me for, but the nurse took 9 different vials of blood. He mentioned MACD, autoimmune problems and allergies. He looked at my skin and scratched my arm and back saying I had dermagraphia and swollen lymph nodes. He prescribed Citerizine (anti histamine) to try to see if it helped at all. He did a Tryptase test which I was concerned about because everything I’ve read says you have to do this test within 2hrs of having a reaction or it’ll most likely come back negative, but when I asked him this and told him I haven’t eaten anything that would cause a reaction in the past 6wks and had been living on boiled eggs, water and broccoli and lost at least 10lbs in weight because of the pain I’m in when I eat anything else and the horrendous diarrhoea I suffer. He said it’s fine I can still do the test??? I won’t get the results for another week, but feel so disappointed. I came away frustrated and upset and no further forward. The anti histamines do help a little with eating but it’s quite random and seems to depend on what I eat, but doesn’t have any marked improvement on my many other issues that would take too long to list. I will tell you the other illnesses I have already been diagnosed with though :-
EDS
POTS
Barrettes eosophagus
Hiatus hernia
Blocked bundle branch in my heart
AVMs in my small bowel and liver
Chronic anemia
Cluster headaches
Osteoarthritis
RLS
GERD
I’m allergic to Augmentin and Erithromycin antibiotics
I’m allergic to the anaesthetic at the dentist (he orders in another one for me which unfortunately doesn’t last as long but stops my heart racing and me passing out)
Ive also struggled really badly with so many medications prescribed by my pain management consultant for my EDS.
My list of symptoms out with these illnesses are at least half, if not more of the massive list you wrote ….
Thanks Corrie
Hi Corrie, I’m so sorry for your struggles and suffering, but… I actually think you got lucky with that consultant, believe it or not. So few even know what MCAD is that to find one who is willing to even run any tests for it at all is amazing! So thank your lucky stars! That said, they were not wrong to run the tryptase now – that’s called a baseline tryptase. It shows how you are doing on an average day for you. Then, they should order (or have standing orders for) another one that yes, you want to get within 2 hours of a bad flare if possible. (Yes, tricky.) Because the majority view is that they will suspect you if you have a rise of 1.2 x N + 2 ng/mL where N is your baseline.
And it’s good he knew to look for dermatographia – that indicates you have a generally high histamine load over all. Which is why the antihistamines will help a little. You might also try (or ask to) an “H2 blocker”, which is an antihistamine for the GI tract (where H2 receptors are in us). These are things like Zantac and Tagamet. You don’t want to take them all the time though if you can help it, as it will lower your digestive ability over time. But ask him about it next chance you get.
I’ve seen all of your other complaints except “blocked bundle branch in my heart” quite common in teh large EDS groups I’m in, so they are not a surprsise to me. Just unfortunate – we really do win the bad health lottery with this condition, don’t we? No system is spared, alas, I’m sorry.
At least you know you’re not alone, not crazy, and… may actually have a pretty good doctor. There is no single easy test, nor any single easy treatment path for any of us with it, though, sorry. So a huge dose of patience is in order. I feel your pain – literally. Hang in there! Glad my writing was some help.
Jan in Portland, OR USA
PS I highly recommend Dr. Afrin’s book on the subject: Never Bet Against Occam, available here in the US:
https://www.amazon.com/Never-Bet-Against-Occam-Activation/dp/0997319615/ref=as_li_ss_il?ie=UTF8&qid=1515647331&sr=8-1&keywords=afrin+never+bet+against&linkCode=li3&tag=disabilitya05-20&linkId=d7852e3718645df6daf541e016d23fe0
Not sure about in the UK – but I’m willing to bet you can get it somehow.
Thanks so much for this tutorial. Have become convinced that very bad health for decades started with MCAS early (dermatographia started age 10, chronic duliarrehea aged6 months to 4 years etc) and then lead to full blown ilness when i had extensive dental work and was “allergic” to several of the chemicals they used, incuding acrylates, eugenol, dycal, bisGMA. I even got elevated badophils from it as i was starting to get sick but docs ignored it. It lead to autoimmune disease which ive had niw for more than 20 years. But in last 4 have worsened with loads of cardiovascular issues i think ate mast cell related including hot flashes and chills, spells of tachycardia and symptoms that hav e mimiced pheochromocytoma. Ive gotten so “sensitive” to every intervention and even touching at docs office causes flares and trying on shoes cause flares
Only thing is i developed very high blood pressure, not low. Also wonder- can low frequency noise be considered vibration? Low freq noise triggers symptoms especially the cardiovascular symptoms and has even sent me to the ER in hypertensive crisis. Trying to also figure out if recently developed “allergy” to milk oroducts of many animal species (cow, sheep, goat, camel,buffalo) could really be non ige mediated. . If i never got the dental wirk i think i would have been fine and the MCAS would just have been a nuicance but would not have ruined or shortened my life. (I actually recovered from first dental assault after about 8 months but the second round. A few laws later was permanantly disabling) anyway, tons of symptoms and chem sensitivities but too much to say here.
You’re quite welcome, glad it’s helping you to connect some dots! Yeah, I’ve started to think of my MCAS as the “Jan behind the curtain” to mangle a cultural reference…
Very interesting and informative article. Thank you for writing and sharing!!
I saw my allergist yesterday for an annual check. (I take a lot of antihistamines to manage my allergies. 2 oral AH, AH nasal spray & steroidal nasal spray, AH eye drops, and have done allergy shots over 11 years. I am doing better but still struggle on occasion to keep allergies at bay.) He discovered a thyroid nodule (I have Hashimoto) and inquired if PCP is following. I inquired about a rash that appears on face and neck (neck redness persists and occasionally itches and has been happening for close to 6 years) that dermatologist (nurse practioner) suspects is rosacea even though no family history and if it could be thyroid related. Allergist has ordered a tryptase blood test. Out of curiousity to see what he might be looking for, I have been doing a little research which eventually led me here.
I do not know if I have MCAD, but it seems as if that may be what he wants to rule out. He also mentioned a possible skin biopsy. My symptoms do mimic many of the symptoms, but they also mimic so many other disorders as well.
It just seems what ever is happening, new symptoms are added with each passing year. (For me my new symptoms are new allergies (meds, food, odors, etc), itchy neck redness that eventually included my face with some swelling, hair loss, have had bouts of syncope for years that they never really investigated and just say probably orthostatic hypotension, GERD, I am finding myself somewhat anxious/panicky at times and a little more frequently (this is new, I have never been like this), I now have a higher resting heart rate and at times (esp during a reaction) and terrible headache. I have periods of extreme fatigue but chalk it up to living with autoimmune disorders: suspected mixed connective tissue disease, suspected sjogren’s, hashimoto, vitiligo, Raynaud’s.
If it turns out to be MCAD…. can be treated, alleviates so many of the symptoms I am dealing with and can reduce inflammation …. I am ready!! There will also be some relief in knowing that we finally have answers.
You’re welcome and glad the article and my writing are helpful! And that your doctor is suspecting and looking into a form of MCAD for you. It sounds like they are wisely trying to rule out mastocytosis (checking serum tryptase level at baseline and during a “flare” or reaction ideally to compare them, more).
I do suspect you of having some form yes, though could not say of course on the internet. But it can be treated, though it may take a lot of trial and error. Remember, sometimes we react to the fillers in our medications too, not just the active ingredients, and vice versa. (So much fun trying to figure this all out, not!)
Anyway, good luck! Glad you found me.
Thanks for all the great info! I started with a Carcinoid dignosis, then Mastocytosis and now Mast Cell Activation Syndrome. I am currently taking Cromolyn Sodium and have mixed results with overall results good. I have responded to the Cromolyn, just not 100 %. One week to my first follow up since starting the treatment. I still worry about the Carcinoid Syndrome, but not to much. Can MCAS become cancer?
Gosh, that’s a tough question – I have seen a lot of cancer in the MCAD groups, but whether the forms of MCAD have any direct bearing on the incidence or not, I don’t honestly know.
I half suspect that having elevated inflammation from any cause can lend to cancer, so somehow it wouldn’t surprise me. But, I don’t honestly know. Glad you found my information helpful. I find it interesting that Carcinoid Syndrome shares many overlapping symtoms with MCAS… hmm… gonna think on this now.
That said, I would at least avoid as much sugar as possible in all cases. (It feeds cancer – and bad gut bugs which lend to many other problems.) Good luck!
After 20 years of being diagnosed with fibromyalgia, yesterday I met with the rheumatologist for the first time in about 15 years and he told me that I did not have fibromyalgia but instead had EDS and MCAD (or S- I’ve seen both). He was probably one of the best doctors I’ve been to in forever (and I’ve worked in the medical system for 20 years, the last 12 or so as an office manager). He was with me for about an hour and a half and he just listened and typed my story in my chart as I talked.
To be told I didn’t have fibromyalgia was not shocking to me. There are times I have wondered about it over the years but figured science wasn’t were I needed it to be at that point. Interestingly, even though it is not shocking, it has been challenging to process the fact that I don’t have fibromyalgia. It’s hard to put my finger on what I find so hard about it but I think the closest thing I can think of is, I’m used to fibromyalgia being the reason to explain my issues and limitations; for 20 years it has been the reason. Now it isn’t the reason anymore. It may sound strange but there is some comfort in it being fibromyalgia. When you look at me there is no visible signs of the things I deal with. In this day and age when you tell someone you have fibromyalgia, people on some level “get it.” It’s a familiar term and they are more understanding about the limitations and issues one has because on some level they understand fibromyalgia. They know there is pain involved even when you look “normal.” Now I have something called Ehlers-Danlos Syndrome and Mast cell activation syndrome. “What the heck is that?” Aaaand you are right back to the status of looking normal so you should therefore be normal. It’s not that I need pity or use it as a crutch, nothing could be further from the truth but I need you to not think I’m being melodramatic when I say that can’t be out in the sun, or I can’t were pants or jewelry because they give me hives; I can’t go for long car rides, and I can’t drive myself (I also have an eye disease), don’t bring that smell near me and don’t whistle or play the bass too loud, I can’t eat that or drink this because it will it will cause me weeks of pain. You may never know these things unless I have to explain why I’m saying No or I can’t. When I tell you I have EDS and MCAS be as understanding as when I said I had fibromyalgia and realize I’m not just being a drama queen or I should just “get over it.” I may look fine but inside my body is at war and it sees the enemy anywhere and everywhere.
P.S. Doctors, when I tell you I’ve hypersensitive to medications, I really AM hypersensitive to medication.
I just had to say you brought me to tears….I soooooo understand and empathize with you for these same reasons. I have a few things people can see, both knees replaced and lower spine rebuilt after car accident at 16 and several other surgeries, but typically I still smile and say I’m OK because I know people can’t really grasp what’s happening inside my body and that beside the obvious pain from tell outward things, there’s so much pain and discomfort and anxiety from all this stuff I’m now being told is my new issues. Anyway, I hope you’re doing alright and appreciate your words as well as this article and just had to say that 🙂
Thanks again!
Ah thank you, I’m sorry you may share this lousy “constellation” of conditions that seem to go together so well yet be so poorly recognized, but am glad you have found a kindred spirit in me. (Hugs.) No, people can’t easily grasp just how much we can have wrong in our bodies with these conditions. Thank God for the support groups who do!
Do be sure to look into the newly recognized Hypermobility Spectrum Disorders and/or Ehlers-Danlos syndromes to explain your knees and spine if you haven’t already. Good luck! [EDIT]: I see from your earlier comment above you’re already up on EDS, so never mind! Just keep self-advocating! (Yes, it gets tiring I know.) Hugs x
Please research CIRS (Chronic Inflammitory Response Syndrome) also know as mould Illness. I have CIRS, so many people are suffering from MCAS because they are exposed to toxic mould in a place where they live, work or frequent a lot. If you look up Dr Jill Carnahan and Dr Sandeep Gupta – Mast Cell Activation Syndrome, you will find a video on youtube talking about this. I need to test the theory if mould avoidance will bring my tongue down, its been swollen for over 5 months. Getting away from mould in a pristine area, no wifi, bacteria etc can help reset the immune system. (I have only been camping once but my tongue swelling did go down.) Mould interrupts the DNA pathway so we get inflammation. Has anyone gone camping in a remote location and found a reduction in symptoms? I know this might sound like I’m a loon but there are other people who have tested the theory and it has worked for them. I was diagnosed with Mast Cell Activation Syndrome by my Dr who was trained by Dr Ritchie Shoemaker in how to treat CIRS. I dont know if my syndrome has progressed to Mast Cell Activation Disease.
Hi Becky, I had not heard of this specific syndrome yet: Chronic Inflammitory Response Syndrome (CIRS), but… I can tell you that indeed, mold (mould) is a huge trigger for the mast cell disease community. And somehow it wouldn’t surprise me if a fair number (or most?) may even be susceptible to this, as I find a huge overlap in primary immunodeficiency issues in my support groups as well. I’m quite sure your hypothesis about leaving the area and staying somewhere dry and safe will help you to know. I’m frequently helping patients to suss out their various chronic environmental triggers, including mold. I just never heard anyone name this specific syndrome as a result. And yes, I love Dr. Carnahan’s work. I follow her.
I myself am sensitive to/react to the penicillin class of anti-biotics and all mold based foods (vinegar, wine) and mushrooms (waaah, they’re so good for us). But I don’t think I’ve had this particular level of trouble – knock wood quick! I have friends with chronic Lyme, so I know just how bad that can be. I first learned about bio-films from one of them about six years ago now.
That said, CIRS won’t cause you to have “primary” MCAS (a form of MCAD) – you would just already have it. But the biotoxins from CIRS would certainly aggravate it and constantly stir it up via the mechanisms I do see described by Dr. Shoemaker here:
https://www.survivingmold.com/docs/UNDERSTANDING_CIRS_EDITV2A.PDF
Let’s put it this way: take two people, one with primary MCAS (a form of MCAD) and one without, and expose them to mold or biotoxins. I’m quite sure the one with MCAS will have a worse reaction and course with the illness than the one without. It’s clear these biotoxins create a chronic inflammatory cascade that becomes pervasive and almost intractable left untreated. But it’s also clear that those with this genetic susceptibility he describes will really suffer. Do they also have primary MCAS? I don’t know. I’d love to find out. I.e, if one could clear up their CIRS (once identified), would they be shown to be sensitive still like all other MCAS patients? Or will some turn out to just be susceptible to mold and biotoxins only? (I’m seeking the Venn diagram here, to be clear.)
My point being, the CIRS won’t “progress” to MCAD as you asked toward the end. You either have MCAD as a primary disease, which would amplify the effect of any infections of any kind, or you have it as a secondary disease to something else. (Mastocytosis, allergies, infections.) The CIRS won’t “cause” MCAD, but it will absolutely inflame the heck out of your mast cells, causing what is essentially the same thing (an inflammatory cascade) secondary to the CIRS. But you may or may not already have been pre-disposed to MCAD to begin with, that’s what I don’t know. I hope I’m making sense! (I think I’m also just repeating myself, sorry.)
Anyway, thank you for bringing this to my attention. I do not think you area loon for doing so. I am no longer surprised by such information and anecdotes. And… I truly wish you good luck with your recovery, regardless. I do think getting away from mold will only help in all cases. You might also like to read my Chronic Constellation post, and see if there is any other overlap there too:
http://ohtwist.com/the-chronic-constellation
Thanks again, and best of luck to you!
Hi, I have Mastocytosis. I have red lesions all over my body from the waist above. My face gets really red from time to time. My triggers are food allergies like nuts and perfume seems to trigger it. Also any scratches to my lesions can also trigger it.
I am 16 years of age and I was diagnosed when I was around 8. They said it would go away during adolescence but I am now doubting that. Any advice whether this will stay with me for the rest of my life or not?
Tough call Jack, as I’m not a doctor. But it is my understanding also that most cases from childhood usually resolve at/just after adolescence. But, for unknown reasons, a small percentage don’t.
I would talk to your doctor(s) about getting tested for Systemic Mastocytosis in your case now because of yours persisting. Tap The Mastocytosis and MC Disease Society for support in this endeavor here: https://tmsforacure.org (including local support groups if any).
Sadly, both masto and MCAS are hard to dx. But masto at least comes with some clear markers usually. (Spots if cutaneous, or concentrations in the bone marrow sometimes, and usually – but not always – elevated tryptase.) Good luck. And keep my resources page handy:
https://ohtwist.com/what-is-mcad/mcad-resources
I’ve had so many of these symptoms.
So many evens slurred speech when I have a attack. Ive been suffering daily since January now how do I get. A diagnoses. My trigger is alchol but I’m currently having issues with drinking so that’s why I’m struggling daily
Hi Amelia, I’m so sorry for your challenges with alcohol. It is truly best if you can forego partaking – it is a known major mast cell trigger. But I understand that’s easier for some than for others to quit. So in your case, seeking treatment for that addiction may actually be your best strategy.
Else, start taking some quercetin and maybe an over the counter antihistamine of choice with your doctor’s permission (if you have one). Always start only one med at a time, and go low and slow until you see if you tolerate that med. (We can and do react even to the meds that are supposed to help us, go figure! Yes, challenging.) Many do well with a daily Zyrtec and Famotidine.
Getting diagnosed is a whole can of worms – this is one of the single most contentious diagnostic processes, and hardest conditions to diagnose for several reasons. INcluding, lack of consensus ON the diagnostic criteria in recent years between Europe and America, and even with consensus, it’s hard to catch a rise in the desired mediator levels in blood or urine for numerous reasons. Many are super sick, but fail to test “positive” for elevated tryptase or urine methylhistamine. But may still respond to the recommended treatment for MCAS: identifying and eliminating triggers (like alcohol), taking mast cell stabilizers and or antihistamines, and for those with forms of masto, controlling their proliferation as needed.
And worse, few if any allergists have even heard of the condition, and few of those are even willing to consider it yet, sorry. (Why I’m posting and tweeting and educating daily, to help raise awareness for all.)
I would try consulting The Mast Cell Diseases Society (TMS) here: https://tmsforacure.org
And also check out these posts by Lisa Klimas that give a little idea about the complexity of the diagnostic process:
http://www.mastattack.org/2015/05/mast-cell-disease-fact-sheet/
http://mastattack.blogspot.com/2014/07/diagnosis-of-mast-cell-diseases.html?m=1
http://www.mastattack.org/2015/04/initial-diagnosis-and-treatment-of-mast-cell-activation-disease-general-notes-for-guidance/
After reading my intro pages here:
https://ohtwist.com/what-is-mcad
https://ohtwist.com/what-is-mcad/when-to-suspect-mcad
https://ohtwist.com/what-is-mcad/mcad-resources
I’m sorry there are no easy answers, and that it is not a simpler process! But, please keep the faith there IS hope and help, especially if you can stop drinking. I promise you’ll feel better! Good luck!
PS If you are drinking for pain, I would also double check if you don’t have an unrecognized Hypermobility Spectrum Disorder also that may be contributing. Also, MCAS itself causes loads of pain, so drinking just makes that back fire. It’s worth quitting, give it a try!
Hello,
I was just diagnosed this past week with MCAS. It is a bit overwhelming. I have diagnosed Von Willebrands disease (see a HEMONC) and a lot of the conditions on your list. Two years ago I was having angina symptoms after exercise, failed a stress test, and ended up having to have a cardiac catheritization. There was zero sign of heart disease, and we now know the burning chest pain and anaphlaxis symptoms were the MCAS. I ended up in ER vomiting and urinating blood- due to during that surgery I had an “allergic reaction” to the contrast dye (Drs couldn’t understand why) and they gave me a lot of steroids that made my stomach lining shred. I also went into anaphlaxis (full blown) coming out of the anesthesia. I started seeing an allergist June 2018… I failed the scratch test (no “real” allergies), but my Ige level was way off and he tested me further w bloodwork and urine. My Drs always suspected an autoimmune disorder, but couldn’t figure out which one .This final diagnosis is upsetting but comforting, because I have something to work with. I’ve started taking zertec + Pepcid daily, carry 2 epi pens at all times. I ordered the book by Dr. Afrin and will start on a low histimine diet. Do you have any other suggestions for me? Thanks!
Phew! What a journey! But so glad you got diagnosed finally, formally! That alone is much too rare. MCAS itself is not autoimmune, but we’re finding autoimmune disorders /diseaseas highly comorbid in the community. Some of us supect it’s because of so much MC activation, the chronic inflammation ends up setting our immune systems into overdrive and they they start attacking self. But who knows. The two do play much too well together in the sandbox, is all I know.
You are off to a good treatment start. I don’t have a lot more to add besides try to identify and avoid as many triggers as you can. Eat as “low histamine” as you can (avoid leftovers, especially fish or ground meats/aged foods, wine, fungi/molds), avoid mold, and I would only add maybe Vitaminc C and quercetin to your supplement regimen if you can. Both help quench the mast cell fires a good bit, such that you may still react, but not go into full anaphylaxis or not nearly as fast and hard, thus being able to self manage at home with or without an epi pen. (Keep them and children’s liquid dye-free Benadryl handy at all times – the latter for sipping when things are ramping up.)
Otherwise, literally keep calm (as calm as you can) at all times, and carry on. And welcome to the club! You’ll get more info and tips from Afrin’s great book, too. Cheers.
Hello! This is a lot of great information, thank you! I was curious to know if anyone had a similar experience to mine…I have hEDS, POTS, and a zillion other things as I’m sure so many of you do too, and about 6 years ago my doctor suspected mast cell was an issue. I have always been hypersensitive to meds, and I have had opposite reactions to antihistamines since I was a baby (they make me bounce off the walls and act erratically) so I never take them. My doctor had me start on the cromolyn sodium ampules and I had a horrible reaction to them, so I had to stop. It’s been years but the evidence of my mast cells making my life worse has only grown exponentially, so I’m going to a new specialist next week. However, I’m quite anxious since the typical treatments make me feel like I need to be tranquilized and put in a straight jacket to avoid jumping out of my own skin. Does anyone else react to them that way? Last time the doctor just gave up on treating it since I couldn’t handle the meds, but hopefully there are more options now that time has passed? I need to be able to eat more than my seven safe foods and not freak out whenever I hear noises I don’t like or smell odors my body rejects. Thanks for any input and regardless, sending you all gentle (virtual) hugs from a safe distance!
Welcome, glad you found this helpful and validating. You are not alone in having the paradoxic antihistamine reaction – I’ve heard of others having this, even though I’m not one of them. I forget why – possibly something to do with cholinergic receptors? I’ll try to point one of my smart friends to this comment and see if they weigh in. You’re not imagining this problem, no and are not crazy. Yes, it makes it that much more tricky to treat the MCAS, sorry!
To that end, I recommend trying OTC Quercetin if you haven’t yet. It at least dampens the reactions about 30-40% I’ve found. So, I still react, but more in a more manageable way.
You might want to look for some online support groups if you haven’t already. They can be a big help. I have an OhTWIST group on both Facebook, and MeWe now – the latter intending to be an alternative to Facebook here:
https://mewe.com/join/ohtwist
Hello,
I fit all the symptoms and am beyond blessed to have a MCAD specialist right up the road. I’ve done some research and am about 99% sure this illness is caused by a boatload of trauma from emotionally abusive parents. I endured sexual assault, every form of emotional abuse known to man, neglect, alcohol abuse, and physical abuse as a child. Just wondering if others have endured the same, if you all can remember.
So glad you ahve a specialist so close by! That’s truly rare and quite a blessing. I have often suspected much the same – I think most of my friends with the worst cases all have really bad trauma histories too. I’m blessedly middle of the road myself, which fits this hypothesis based on my childhood experience. (Neglect, and verbal abuse, witness to physical abuse, no sexual abuse thank God as a child, left to raise myself mostly.)
But I also wonder if Chiari or CCS lends too – it seems like those who have impinged CNS (hind brain, more) seem to also have the twitchiest mast cells. Almost like it’s a survival response. Those with both may just be semi-doomed, sigh. 🙁
Dear All,
I am a third year student of orthomolecular therapy and in the course of doing a review
I learnt about the connection of mastcells, adhd and autism, which already sparked my interest. I have a son with these diagnoses. I then made the connection myself of allergies running in my family, but also hypermobility (not severe, i always considered it just my body type). Additionally my mum has reumatoïde artritis and i some signs of osteoarthritis (which nowadays is recognised not to be wear and tear but also an inflamed situation). Yesterday i came home with a diagnosis of mitralisprolaps (weakening of one the heartvalves) and started googling some more, because that seems to occur more frequent in individuals with a form of reuma (hypermobility is considered in the reumatic space if i am correct).
Anyhow just prior to finding this site i had been puzzling elements together myself of the involvement of mast cells in all these ailments running in my family and foundation this term MCAD. I live in the Netherlands and i doubt whether any physician has ever heard of it.
To get to the point finally: potential treatment options!.
During my review i learnt that Italian researchers have been treating autism (because they link it with mast cell overactivity) with a combination of the ultramicronised forms of PEA-Luteoline (both completely natural substances, and ultramicronised for being able to pass the blood brain barrier better). Both substances are claimed to dampen mast cell activity and PEA in particular inhibits the inflammation systems that has gone in overdrive. Luteoline is a flavonoid like quercetine. Luteoline is ‘fatloving’, so better suited to reach the brain for local mastcells. Quercetine, also mentioned here more suited at peripheral mast cells. So i figured to look for ultra micronised PEA-Quercetine………which apparently exists (in a study anyway)!!! Still trying to source it though.
These substances that i just mentioned i really worth looking into i believe. The are natural and most regular physicians will probably not know of them though.
Good luck to you all on the Journey to relief.
Cheers, Xandra
Thanks so much for writing, Xandra, and for going into medicine! We need more of you! Yes, I’ve heard of both quercetin and luteolin benefiting MCAS patients. Leading researcher and pharmacist Dr. Theoharis Theoharides (Theo for short, smile) even developed his own line of products that a separate non-profit markets on his behalf so there’s no financial conflict of interest. Maybe yhou’ve already found them: Neuroprotek and Fibroprotek are a couple. (I have no financial connection/gain from mentioning this.) And yes, many autistic friends have benefited from PEA. I gave it a whirl last summer, but reacted. I may try it again “just in case”, but I was bummed – I seemed to feel worse/more flared than without it. (I”m on a fairly high amount of quercetin daily, plus H1 and H2 blockers and trigger avoidance.) We’re all so different, and one man’s panacea is another man’s trigger, sigh.
I usually recommend trying single ingredients for this very reason: if anyone is going to react to something, it is us! And, if you take something with multiple active ingredients (never mind the inactive ingredients too), it can be super hard to detect just which part is making you react/sick. But, if you can take the combo, and find one you like, go for it!
You are totally on the right track. And I’m so glad you stumbled onto this information and healing path. Good luck to you as well!
I’m thrilled to find your site! I diagnosed myself (after the Dr. didn’t) using the Internet while in England last year where I have no health coverage. I started taking cetrizine and famotodine which controls my generalized pruritus and diminishes the “bladder” pain but not enough. I’m a 72 year old retired RN who developed interstitial cystitis which I also diagnosed after my gynecologist ruled out other diagnoses. She finally agreed with the IC diagnosis. I also have several other symptoms of MCAD. Lab blood work is all normal. Microbial UTI was ruled out twice over the last 30 years; the dr. blaming my cystitis pain on low estrogen. I’m realizing the food triggers are a problem and I’m trying figure out what sets it off. I’ve had a history of IBS and GERD for 15 years more or less. I’m hoping to return to US and get referred to an immunologist hematologist Dr. knowledgeable in MCAD. Hopefully Medicare will cover it. I’m hoping to get NHS insurance here since I’m permanently here. Has any research been done on the familial incidence of MCAS MCAD?
Thank you ??
You’re so welcome, I’m glad my site could help validate your personal feelings and findings so far, even if your doctors can’t or won’t fully. (You’re in good company and lots of it unfortunately.) Many of us find we can manage much of our symptoms ourselves with over the counter remedies and meds like you’ve done. I would just add a suggestion to try some quercetin too to help keep the reaction levels (histamine) down even more. (It’s another OTC natural mast cell stabilizer that helps quell inflammation. There was even a run on it last year due to COVID when it came out that it can help stave off cytokine storms.)
As for research on the familial incidence of MCAS, yes, actually, one study ended up smoking out a duplication of the gene for tryptase, that helped explain a phenotype called “Hereditary Alpha Tryptasemia” now (published in 2016, I was actually part of the double blinded study, though I still don’t know if I have it, i need the money to pay for the now commercially available test). Alas, that still only explains a very small subset of us, and indeed many of the best specialists like Dr. Afrin are observing MCAS to run in families, but there isn’t any more research out yet to back this. I think I read that there are hundreds of KIT mutations, and so far we’ve only characterized a couple, with the best known being D816V, which is associated with some forms of mastocytosis. (It seems to lend to the little buggers overstaying their welcome even in the absence of stem cell growth factor.) But nothing definitive yet for “just” MCAS, which, much like hEDS may turn out to involve several mutations and/or genes. We could use a lot more people studying it for sure. Here’s a bit on the HATS result:
https://www.nih.gov/news-events/news-releases/nih-scientists-uncover-genetic-explanation-frustrating-syndrome
You might find some more answers on my Resources page here too:
https://ohtwist.com/what-is-mcad/mcad-resources
I truly hope we get more studies done soon!! Too many patients are twisting in the breeze and being dismissed without definitive biomarkers (elevated mc mediator levels) despite being super sick and responding to the therapy for treating MCAS. Which I also wish they would rename “MCOAS” for Mast Cell OVER Activation Syndrome. Since everybody has some mast cell activation or they’d be dead! And it’s the over activation (or “inappropriate” activations as Afrin calls it) that is making us so ill. Anyway, huzzah for answers, and hopefully you’ll continue to dial in your meds and get even better results over time. (Don’t give up, it’s loads of trial and error for all, sorry.) Cheers,
Jan
What about all the accumulation of mast cells and fibroblast activation. My triggers are mainly heat, and psychological stress. When It started I noticed my blood pressure dumping and then I would have drop attacks which progressed to fainting seizures, turning purple, flushing, but the constant has always been the labile and volatile blood pressure and tachycardia. Two strokes Teo heart attacks, doctors telling me I’m seeing things, it’s been a long journey since 2006. I had mentioned mast cells to xxx major clinic and cytokines storms, and was told I would know if I was having one, or had it. I said well what about my purple feet? It seemed to follow a psychological stress pattern although the fainting and seizures included heat. I was abused as was my son which is when this all began, it was an overload of some sort. They would tell me my blood pressure was low because I took it too much, well when your MAP is lower than the number it takes to support your body’s blood oxygen requirements, and doctors don’t like intelligent patients. I had MRSA after a bout of Cellulitis, but in between constipation and an intestinal infection that my doctor wouldn’t treat, (a year later a different doctor confirmed that I actually did have systemic MRSA, which then triggered where I am now, a year long daily triggered episode of MCAD, my kidney levels are high my liver levels are high issues with my bile duct my lower lungs, non productive cough, fibroblasts in my throat, mast cells just everywhere head to toes fibroblasts and loose connective tissue nodules or clumps, it takes me an hour to wash my face, two to shower, and it’s back in ten minutes, my blood doesn’t coagulate I have bruising I don’t know how, and now tiny pinpoint nodules everywhere, and when I itch, it’s maddening. The mast cells just settle into the grooves of my skin, and then the fibroblasts, it’s as if my skin is falling off. If I don’t put tea tree oil on, oh boy. It’s in my nose, my eyes, eyelids, every nook and cranny, when I saw my ring to on my left foot look as if a tight rubber and had been on it and then noticed that it was a clumping of loose connective tissue, I said that’s it. I start low level blue light therapy three times a week for three months on Monday, but it’s been known to speed the immune system up in some patients ba slow the immune system down. It’s just recently been approved for use on cancer patients because it’s cheaper and can be done more often than the typical radiation treatment but for MCAD, there’s opposing views for the reasons I mentioned, but I have concerning, (kind way, or medical lingual for probably cancerous), lesions., so this will only deal with those, if it’s successful. It’s a standing booth full body treatment. What comes next? Will they do a bone marrow biopsy to see if I have an overproduction there? I heard that’s the only real hope is a bone marrow transplant., but how long do they wait, Id rather do it now than when all my organs are failing. If there’s any doctor out there that can help me, please call me 402-601-6354. I am in misery 24/7, I have no support to speak of. I’m a 57 year old woman, with her 7 year old Maltese Yorkshire Baxter whom I can no longer walk four times a day, thank God he is so very patient. He is all I have, and I worry what will happen to him when I’m gone.
Hi Simone, I can hear and feel your pain in this comment on my post. I’m so sorry for your misery. That said, I want to clarify a couple of things / some terminology:
a) you cannot see fibroblasts with the naked eye. They are part of what makes up our connective tissue, inside of us. So your comment that you can see “fibroblasts in my throat” is a bit misleading. I’m going to guess you meant “fibers” (or similar) here, and if so, I will also add that I believe you. I know people with something called “Morgellons” which is highly controversial in medical circles unfortunately. And I’m suspecting this may be the case for you based on your description. Here’s some info on that:
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5811176/
And I will also note that virtually everyone I know with Morgellons also has a primary scabies or mite infestation of some kind as well which almost all dermatologists and doctors will fail to recognize or will outright deny. (The bugs may be spreading the Morgellons in fact, but science isn’t clear on this.) But because they are microscopic, it is really hard to prove this. And again, that is in addition to lesions, fibers and other things found on the body with this infection. Which, like any infection, will also set off your mast cells, alas. I say this as your description matches that of some patients who have this I’ve seen.
Some info on fibroblasts:
https://www.practicewithpronouns.com/#/?_k=v1i8t3
b) you also cannot see individual mast cells with the naked eye, so the comment about them “settling into the folds of your skin” is also a bit confusing/misleading. (Unintentionally.) That said…
I believe your suffering is real. I also suspect you have a form of MCAD as well as some other things going on but I cannot tell or help you sight unseen – no one can. The BP drops and purple feet are pretty common in people with MCAS and dysautonomia – my reactions make my BP drop. Often our blood pools in our feet too if we have comorbid connective tissue disorders like Ehlers-Danlos syndrome or the newly described Hypermobility Spectrum Disorders to. This is a form of dysautonomia. In white people, it makes our feet look purple or blue. Black and brown people experience this too – I just don’t know what color their skin turns on their feet, but I expect they become darker. (Just to be clear.) I apologize for my ignorance of same as a white person.
Some more clarification: everyone experiences SOME mast cell activation or they’d be dead. Mast cells are literally our first line of defense in our body’s imnmune system. (The Primary Immune defense system.) And, all mast cells respond to the protein coats of viruses and bacteria via their toll-like receptors which is why we so often struggle to know if we have a cold, or “just allergies”. (Not that allergies are any cake walk either, heh.) Anyway, that’s why we often take antihisamines with our colds and flu. To tamp down that part of the reaction and resulting symptoms.
People with MCAS have extra or “over-active” mast cells (I wish we’d rename it Mast Cell Over-Activation Syndrome for this reason, but don’t listen to me) which go off in response to many non-proteins, like scents, pressure, stress (of all kinds, physical and especially emotional trauma), vibration and sunlight. I absolutely believe the stress of your abusive past was a trigger for a sort of onset cascade, I’m so sorry. This is not uncommon in us either. Like, even if we had mild issues prior, suddenly things ramp way up and we react to so much more, and yes, including stress and trauma, alas. I’m so sorry. (I hope you’re in a safe place now.)
My best advice for you would be to try to find both a) a local support group to you (hold that thought) and b) a savvy naturopath who recognizes and understands MCAS and other infections. All infections will lend to increase in mast cell activity. Chronic infections like Morgellons definitely will too, if that is what you have.
I’m guessing you are in the US based on your phone number. Regardless I will refer you to both of these organizations for help finding support groups local to you who can help you find local doctors (if any) who may be able to help:
a) The Mast Cell Disesases Society: https://tmsforacure.org
b) EDS Awareness (aka Chronic Pain Partners): https://chronicpainpartners.com (alternatively https://edsawareness.com)
I dearly hope you can get some relief and help, one way or another, whatever you have. I do suspect you of a mast cell disorder of some kind, as well as some kind of unknown acquired infection. Staying as calm (zen!) as possible (ha, not easy), and low histamine as possible will only help. I avoid ground meats, and all leftovers to this end now. Especially fish. (Fish is super high histamine.) Also avoid alcohol, sugar and fermented foods. I also take daily antihistamines to help keep my baseline histamine level down. This helps lower reaction levels over all. (I never need to use an epi-pen and get by with children’s dye-free liquid benadryl in an emergency.) Good luck.
PS When Else to Suspect a Hypermobility Spectrum Disorder or form of EDS in case that helps too: https://ohtwist.com/when-else-to-suspect-ehlers-danlos-syndrome
It’s crazy, my own boyfriend told me it was just a panic attack when my heart started racing, and I felt like I was going to pass out. All I was doing at the time was watching tv. Then the cardiologist thought it was supraventricular tachycardia. Then I started having vertigo, the soles of my feet were itching so badly at night I couldn’t sleep, and my lips started swelling every morning. Now they are swollen almost constantly. I am currently getting tested (24 hour urine) for MCAS. I already went through allergy testing, testing for lupus, and other autoimmune disorders. Everything fits with what I have been going through.
Well, you can kind of see how it can highly resemble a panic attack! I actually strongly suspect many so-called “panic attacks” that present in the ER are possibly MCAS reactions no one yet recognizes as such. We can and do tend to have co-occurring anxiety, but this keeps being a red herring.
I’m glad you persisted and are able to drill down and test for MCAS. That said, know that the testing is notoriously inaccurate (many false negatives) but, the fact they’re even willing to consider it is great. And, try for a working diagnosis if that happens (you’re negative for any elevated mediators they seek) – there’s not a lot of harm in trialing some anti-histamines and a mast cells stabilizer like quercetin. I actually did this on my own once I figured it out, and self-treated for years before I finally got a doctor on board. I’m still technically negative, so only have a provisional or working diagnosis yet too. Many of us have to -it’s the best we can get.
Anyway, good luck! And I strongly suspect you have this too from your description. I hope you get some helpful treatment ultimately.
I suspect that the reactions being attributed to vibrations (i..e, car, motorcycle) are actually induced by the gasoline fumes (Petrochemicals). Read Dr. Theron G. Randolph’s papers. He was practically destroyed for claiming there was a major “Petro Problem,” ala the AMA and Petro industry. Petros are probably one of the main MCAS triggers in the it is ubiquitous (i.e., contained in 99% of pesticides, many pharma drugs, etc.).
I don’t doubt the fumes play a factor, but I promise you, vibration itself absolutely sets my mast cells off without fail. Including inducing ganglion cysts in my wrists back when I used to mow lawns. And, in non-gas powered vehicles. The vibration of the road itself lends.
So, both, and.
Hi, I have hEDS so knew there is a link, when my symptoms started to really scream (I was having trouble breathing) I eventually went to the GP. I told him my suspicion of MCAS and he looked at me as if I was speaking a foreign language. Ok we’ll look at that later but first we need to sort out your breathlessness! I went for all the respiratory and cardiac tests (they discovered CAD) but that really wasn’t the problem as far as I felt, I struggled to catch a breath but had no problems breathing out. A few months later and boy did my hives go wild and it seems if I’m hot (most of the time) and sweaty and put my arms on something the rash goes wild, I have at times made myself bleed from scratching as had no access to antihistamine at that occasion! I needed to go back to GP and saw a paramedic who instantly recognised the potential of it being MCAS as she has POTS and knows about hEDS and MCAS – well knock me down with a feather!!! She actually had to tell the GP’s at the pre surgery conference all about MCAS so they knew something about it. When she told me this I sat and cried and she smiled at me knowingly and said you don’t have to fight to prove anything all the symptoms you display are classic MCAS, she’s referring me to dermatology as they are the ones to diagnose it in the UK.
I do want to say that vibration is by far one of the most problematical for me! I cannot use an electric toothbrush because the vibration is so high in my mouth that I nearly pass out before the rest of the histamine kicks in. I also break out in a rash just pushing a supermarket trolley! So I definitely agree, no fumes required for my symptoms to be triggered!
The one thing that I’d probably the hardest is actually knowing your having a reaction to something that was perfectly ok yesterday and will be perfectly ok tomorrow – it’s a rollercoaster!
Oh I’m so sorry you suffer so badly from this lousy co-occurring condition, Susannah, but I’m SO glad you stumbled on the answers with the help of that great EMT and my blog!
It is very alarming and distressing how few doctors yet know about it, and then how little they do even among those that do. There are some narcissistic gatekeepers even among the specialists that lead the conferences, who I watch deny others lived experiences every year, sigh.
Anyway, yay for answers, right? And knowing you’re not crazy, not losing your mind – just your mast cells! (ha!) Definitely find some antihistamines to help you (it’s an individual process, and y es, we can even react to the fillers in the tablets if not the active ingredients themselves sometimes too – go figure!). Quercetin (an over the counter supplement) can help a bit too. (I feel like it knocks the amplitude /severity of my reactions down a good 30%, even though it doesn’t eliminate them fully. But this keeps me functioning more than not along with all else I do.)
You might like this post next if you haven’t yet seen it: Finding Your MCAD Triggers
So my 13 daughter was just diagnosed with hypermobility possible EDS when we started pt for a grade 1 spondylolithesis. For years I could not understand why she always looked so bloated (like she was on steroids ) yet her diet and exercise levels did not align with her weight and size . She’s a dancer and was dancing almost 20 hours a week . She was in and out the hospital as a young child with bad asthmas attacks, then she was diagnosed with cold urticaria when she went anaphylactic one day at the pool. We had her tested for all kinds of allergies and the only thing that showed up was dairy . We’ve pulled out diary and gluten from her diet and that has helped tremendously with the bloating but she still gets it time to time and brain fog as well. I still feel like we are missing a diagnosis somewhere that’s causing all this . What are your thought s??
Well, Of course I’m not only not a doctor, nor am I her doctor, but… what you describe fits right in with the common experience of many with MCAS. Though hat tip for removing gluten and dairy – most of us do benefit from doing that. But, knowing what else I know, I would also be sure she got a thorough endocrine workup, and rule out hypothyroidism. Side note – as I wrote here years ago, you can be hypothyroid even with a TSH level in range.
Not only is the range too wide per some doctors, but, even if you test well in any range, if your liver is compromised and not functioning well, you may not convert T4 to T3 (I think it is), so this renders it still unavailable to the body. In other words, it causes a sort of secondary hypothyroidism most doctors won’t recognize for what it is because they just stop with the TSH. Few regular GPs (MDs) recognize this. I would seek out either a naturopath (ND) in the US, or a functional medicine doctor (MD) wherever you can to explore that, if you don’t get anywhere with regular western medicine wherever you are.
But otherwise, yes, she sounds a lot like an MCAS patient. Brain fog is a huge part of it, sorry. So slowly finding and eliminating her triggers, and maybe adding an antihistamine or two, and some quercetin might help. But, ideally, try to see an allergist/immunologist who is willing to recognize MCAS. (Yes, a medical unicorn, sorry.) And know that diagnosing MCAS itself is quite hard, few get a full official diagnosis. (The doctors are very gatekeeping of this for some reason, reserving it only for the very grossest and sickest of cases that are easy to get test results for, leaving the rest of us to flounder and get a provisional or working diagnosis at best.) I mostly self-treat myself. And I can’t dodge all these symptoms. That’s why I’m on disability along with my disabling EDS and pain. Hope that helps.
I have had a strange illness for the last 8 years which was diagnosed as lyme, babesia, FND, chronic migraines. I adapted and accepted my symptoms, but two years ago I was sat watching TV, eating pizza and all of a sudden my vision went funny, my heart raced and felt strange, and I had severe confusion. I was taken to ER where I subsequently lost my speech, couldn’t understand what they were saying to me. After 4 hours I could communicate again but I was unable to spell/read for a day or two. It was the most bizarre scary thing that’s ever happened….. anyway that was the start of a new phase of my illness and I have suffered and experienced symptoms that I didn’t think were possible. I’ve been struggling ever since just to exist. I’m wondering if this could be MCAS. I seem to react to all new meds, foods etc with so many symptoms. What’s the go to test to diagnose? Tryptase?
Ack, I just lost my first really excellent longer response to you due to an internet glitch, waaah. So let me quickly respond in reverse order. MCAS is really hard to get properly fully diagnosed. There is no single easy test, and the tests there are, are onerous to get, and often give false negatives. Many of us end up with a “working diagnosis” or presumptive diagnosis for this reason – we may not pass the (few) tests presently recognized as pathognomonic for MCAS (disease causing). Some insight, bearing in mind that MCAS is a diagnosis of exclusion:
https://www.mastattack.org/2015/04/initial-diagnosis-and-treatment-of-mast-cell-activation-disease-general-notes-for-guidance/
http://mastattack.blogspot.com/2014/07/diagnosis-of-mast-cell-diseases.html?m=1
https://www.degruyter.com/document/doi/10.1515/dx-2020-0005/html
Thing is, few doctors recognize the condition even yet, there is not global consensus on the diagnostic process as yet, and, the tests are notoriously often false negatives. So don’t let that (all) discourage you.
Do I suspect you may have MCAS based on the above? Yes, possibly. I’m not a doctor, nor yours, so could not at all say for sure, but I do think it’s worth investigating, yes. Just, think marathon not sprint, and bring three truck loads of patience to the process. Hope that helps.
PS A quick poor man’s test: start taking a daily over the counter anti-histamine of choice (carefully, with doctor’s permission) and see if these episodes reduce or become less severe. Ditto trying daily quercetin, a known OTC mast cell stabilizer. (Always only try one thing at a time, in case you react, because yes, we can react to ANYTHING including antihistamines and medications safe for most folks. This can include just the fillers or dyes used too, so be careful before writing off a drug – try compounding it safely first.) A food and med journal may also help you start to identify more triggers and avoid them.
And then, trying some Benadryl (if tolerated) during these episodes may help too. Definitely talk to a / your doctor. You may want (probably should have) an epi-pen handy going forward. I highly recommend joining a support group online if can on this journey. It’s a tricky one. Check out https://tmsforacure.org for more support.
Hi,
Great post! I’ve been suspicious that MCAS is part of a number of the weird, random “allergic” reactions I’ve had. I check almost all the points you’ve listed above. Many things have been ruled out, but now to get a doctor to actually diagnose this.
I’ve also came across this and thought that you might like it and it might be a help to others.
https://mastcell360.com/mcas-resources/
Thank you for the reminder – Beth’s site is a fantastic resource. I thought I had it on my resources page but it appears not. (I also could stand to strip down my resources page and break it into several subpages now like I did my EDS Resources page – so many to sort through!)
Anyway, yes, and glad I could help you to suspect. That said, re- diagnosis, don’t get your hopes up. Very few doctors will formally diagnose MCAS even if you have ALL the signs and are very sick. First off, because very few recognize or believe in it, secondly, because, if they are rigid rule followers, it’s still hard to pass the pee tests required (show signs of elevated mediators even during a flare).
But, if you can even get just a provisional or “working” diagnosis, that will help, as they can and should then help you to self-treat with things like antihistamines (yes, you can get most over the counter now), but also some mast cell blockers like Cromolyn Sodium for the gut, aka “Gastrocrom”, or other forms. (Opticrom and Nasalcrom are over the counter in the US now I think at least.) But also Ketotifen. And more.
Good luck!
Yes, a chameleon!!!! Great choice and I’m with it 🙂
Cheers!
I was fortunate to work with a nurse that was empathetic and helped me figure out what I was dealing with. None of the general practitioners treat patients with MCAS here. There have been several holistic clinics popping up in our area that don’t accept anyone’s medical coverage. These places treat MCAS, provide weight loss assistance, etc. So at this point, I’m on my own. I’ve tried several things based the research that I’ve done. Nothing has helped so far. Since September of 2024, my right foot has been has been severely restless. I had a hotdog at a football game and I continue to pay for it. I don’t pack my lunch for work, so I’m hungry daily. I am quite literally afraid to eat. I have started a walking regimen. Sweating usually causes severe itching and hives, but it isn’t hot in Southeast Missouri yet. If anyone can share advice, I’m all ears!
I’m so sorry for your lack of proper medical care where you are. This is an all too common experience yet. And even with medical care, it’s still pretty much a trial and error experience: going through all the various antihistamines to see which ones you tolerate, and can help. Ditto any mast cell stabilizers (not many). Getting a positive diagnostic testing restul for MCAS is extremely hard, so good doctors are going ahead with presumptive diagnoses and treating anyway. You can do a little bit on your own with over the counter meds. Always start low and slow – only one med (or even food) at a time, wait at least a week before adding another, to see if you react. And if you do react, mind that you may be reacting to one of the “excipients” (fancy word for fillers), and not necessarily the active ingredient itself. Yes, arduous! (Some folks get their medications compounded with safer fillers for them, like rice flour or potato starch. Expensive, but worth it if that’s the only way you can take them.)
Also, try to avoid high histamine foods in general, which includes sausages and ground meats of any kind, yes, sorry. Fresh, organic foods are your friend. Try freezing leftovers, but even that is no guarantee. Avoid fermented foods, wine and aged cheeses (all high histamine). Quercetin is a decent natural mast cell stabilizer sold over the counter. It knocks my reactions down about 10-20%, which combined with anti-histamines and careful diet keeps me out of the hospital and away from my epi pen most of the time. Be sure to check out my MCAD resources page for more, and join The Mast Cell Diseases Society for more support too at https://tmsforacure.org