For Doctors
Below please find the latest and best resources for doctors for getting quickly up to speed on everything to do with Hypermobility Spectrum Disorders (HSD) and all forms of the Ehlers-Danlos Syndromes (EDS).
EMERGENCY TREATMENT INFORMATION IS JUST BELOW THIS BRIEF INTRODUCTORY SECTION
This information is subject to change over time. Notify me at info@ ohtwist dot com with questions. It is compiled from my personal observations of thousands of patients (over 100,000 across hundreds of online groups and Twitter) over the last ten years online on Facebook and Twitter and MeWe and Mastodon. As well as of hundreds met in person as a support group leader since 2012. And many doctors who follow me (and I them) on Twitter and elsewhere. I keep it as up to date as possible at all times. LAST UPDATED October 9, 2025
So while there may not be studies available backing up all of these observations yet because science takes time and always lags (always), you can think of me as a “reporter from the field” if you will, giving you some key pointers based on my semi-photographic memory of thousands of posts online.
I was tapped as a co-author of the EDS Toolkit for Doctors published in 2018 for this reason. Which I highly recommend for any doctors seeking to diagnose a NON-EMERGENT patient in front of them regardless of my involvement – it was spearheaded by General Practitioner, Dr. Emma Reinhold for fellow Primary Care Physicians.
NB YOU DO NOT NEED A DIAGNOSIS TO TREAT US PROPERLY IF YOU SUSPECT A HYPERMOBILITY SPECTRUM DISORDER OR FORM OF EDS in an unidentified or undiagnosed patient. Better safe than sorry. Don’t spend time on the Toolkit above if you’re in the ER. Save that for later!
NB Opportunities to receive CMEs and keep up to date with the latest in the field of hypermobility spectrum disorders and EDS are listed at the bottom of this page.
PRESSING CONCERNS FOR EMERGENCY CARE
IN CASES OF EMERGENCY IN KNOWN OR SUSPECTED HYPERMOBILE OR EDS PATIENTS:
- HANDLE WITH CARE we can injure just laying “wrong”, e.g. on our sides, or being pulled up by our arms. (I can literally move my own skull on my own spine with my own hands, e.g..) We may also be super sensitive autistics. Be gentle and ask first, whenever possible! We may also bleed or rupture vessels easily, and need help restoring blood volume before you try to get a vein.
- MEDICATE BUT BEWARE of unexpected outcomes and reactions! (We tend to have unexpected paradoxical reactions, requiring either much more or much less of a drug for the desired affect. And we can react to literally almost anything, e.g. glucose in an IV, any and all adhesives, fillers, dyes, etc.) Every single patient is different, so you cannot generalize much, sorry! Just keep an open mind and be ready for unexpected reactions thanks.
- WE MAY NEED MORE ANESTHETIC than the average patient. And may wake during surgery, even if you can’t really tell this has happened. (We seem to process it much faster than other people.) Please believe us if we report it, thank you. (See a popular and effective dental numbing formula below.)
Assume all patients have vascular Ehlers-Danlos syndrome (vEDS) until and unless told/shown otherwise. This includes patients with Hypermobility Spectrum Disorders and HMS, JHS and BJHS also. Many are mis- or under-diagnosed with “just” HSD or hEDS. And some properly diagnosed with HSD are even more severely affected than some EDS patients, but just don’t happen to fit the current rigid and narrow EDS diagnostic criteria. Better safe than sorry, truly. (Learn about all the types of EDS here if not emergent.)
The EDS v. Hypermobility Spectrum Disorders continuum reflects differences only in rarity, not severity.
EVEN IF WE DO NOT HAVE diagnosed vEDS, proceed with caution – we are all prone to increased ruptures of soft inner tissues and organs, easy bleeding and bruising and blown veins and artery dissections, poor suturing, subluxations and even full dislocations on the surgical table or during transfer, CCI and AAI, IIH, CSF leaks, strokes and aneurysms, aspiration hazards, paradoxic medication reactions, increased pain/poor response to the “caines” (novacaine, lidocaine, etc.) and/or low pain sensation (may be grossly injured but not demonstrating pain as expected in proportion to the apparent injury).
And most of us are neurodivergent in one or more ways – either Autistic, ADHD, or AuDHD (yes, both, really and more) and experience all that that entails, including often being quite traumatized by “normal” life that may not bother you.
Practice trauma-informed care as much as possible accordingly, even if you aren’t sure it’s necessary. This will frankly benefit all of your patients, not just autistic ones.
Not all patients are equally hypermobile even within the same family. Nor will they all behave or present alike. In fact, not all with EDS are bendy – some of us stiffen greatly with age, secondary autoimmune diseases and arthritis and injuries. And some never are, even from birth. In fact, some people are born stiff. (Ask Dr. Jaime Bravo about that.)
Please believe us and do NOT force us to perform the Beighton 9 point scale or ANY of our bendy “tricks” for you – this can cause serious and irreversible harm. There are plenty of other ways to suspect a CTD. Here’s a handy website for doctors IN AUSTRALIA ONLY for now to help score hypermobility (2025).
Top tips gathered from OhTWIST followers (patients and doctors):
- Avoid Cipro and all the fluoroquinolone antibiotics whenever possible*. They pose a tendon (connective tissue) rupture risk for everyone, but especially for hypermobile people. (We probably generated the black box warning on them.) *Yes, I realize sometimes they’re a last life-saving resort, which is why I did not say never use them. Just, keep them as that very last resort if at all possible thanks. Floxing is very very real. Alas, sepsis is also very real and also semi-common in us due to comorbid PID. Just exercise great caution with this drug class, thank you.
- Anesthesia – we often need much more than expected or additional “topping up”, and may literally wake during procedures, or partially awaken and feel everything, but remain paralyzed and suffering while unable to tell you. We also often get little benefit from the “caines” (novacaine, lidocaine etc.) often needing much more than expected. This may be due to hyper-adrenergia causing us to out-process them too quickly. (See the Dental Freezing Formula below for dental procedures.)* We may also REACT to almost any anesthesia. (See next.)
- We may react in unexpected (paradoxical) ways to any and all medications, adhesives and anesthetics, and often need much more or different pain meds than typical. We are not drug seeking! We have differences in metabolism of medications (some are super fast, some slow), and may also react to any and all medications in unexpected ways due to our comorbid Mast Cell Activation Syndrome (MCAS), diagnosed or not.
- We may experience atypical anaphylaxis due to our highly co-occurring MCAS diagnosed or not. And, in reaction to almost any substance, even some you think are truly benign. Not all anaphylaxis is throat closing. Some have extreme BP drops only, others spike super high, then crash hard, some never have skin signs. Some have extreme mood swings or changes or extreme irritability. Expect anything and keep epi and Benadryl handy. Consider a Benadryl drip during or after surgeries.
- Many of us do better using butterfly needles for placing IVs, and beware of easily blown, dodgy veins. (Please don’t dig around or keep trying. Just use a butterfly needle instead, thanks.) We also bruise and injure quite easily – double check the family for hypermobility before removing children. And our skin may rip or tear very easily, especially when removing tape. We may need steri-strips in addition to sutures to hold us together. And can react to many tape adhesives. (Yes, tricky, we know.)
- We may need more fluids than most, or more than expected (dehydration is common and also worsened by MCAS which flares with pain and stress). This will help stave off/reduce POTS flares too. But plain drinking water will just go through us without sufficient magnesium especially, as well as potassium and sodium. (Hypokalemia is not uncommon in us for this reason among others.)
- We may not “perform pain” as you expect either – either being hyper or hypo sensitive, or, sometimes just not showing it in our face or voice, but still feeling it. Or, we may express it in unexpected ways including laughing. Please believe us when we tell you we hurt, thanks.
- Be careful intubating – avoid using any forceful positioning head thrusts, as we often have cranio-cervical instability (CCI and AAI) and are also prone to strokes and aneurysms, and literal dislocation of our cervical vertebra, as well as all forms and manifestations of TMJ from dislocated jaws. (I can move my own head on my own spine with my hands at will, no joke.)
- We are also prone to spontaneous CSF leaks anywhere along our dura, including the spine. Consider using fine pencil point needles for Lumbar Punctures, and avoid unless really needed.
- Perform CPR carefully on us and only if you have to – you can easily sublux or break our ribs and leave us with lasting injuries and damage. (Yes, I know, you’re just trying to save our lives, but still!)
- MRIs beat CTs, which beat X-rays: Many of our very real, painful, soft tissue injuries can only be seen in MRI’s, not CTs or x-rays. Consider getting an MRI for the patient if they are still complaining after you find “nothing” with the other two imaging systems. Try not to dismiss us too quickly because you can’t easily “see” something wrong, thanks. (Even if an MRI is negative too.)
- Medical PTSD is real. And a much too common experience for us, especially the more autistic among us. Many of us have been fobbed off, gaslit and mistreated for years. Thanks for bearing with us if we lose it on you. Help us to educate your colleagues to help avoid this in the future. (Why I’m writing so much!)
*Dental Freezing (Numbing) Formula that works great for many patients with CTDs:
1/2 mepiva w/out epi, 1 art w/epi 1:100,000
“art” stands for “articaine”.*
*articaine and bruvidicaine has worked well for some CTD patients too
Reference: dental numbing, dental freezing
Pain is also a mast cell trigger, as are temperatures (hot or cold, not always even extremely so thanks to dysautonomia) and stress (bright lights, beeping machines, loud voices, chaos, poking and prodding, more). Mast Cell Diseases (all types of MCDs, diagnosed or not, formerly termed “MCAD”, but now MCD since 2023) lend to increased dysautonomia and fluctuations in body systems beyond typical range.
Please see my MCAD Resources page for more on that and consider treating for mast cell reactions along with pain. (Or listen to and believe us when we say we need to, or ask you to thanks.) Many patients will benefit from a Benadryl drip in their IVs during or after surgery, even if not diagnosed with MCAS or Mastocytosis. Especially if in pain.
One EDS family was found to have a voltage-gated sodium channel defect lending to their experience of complete failure of all local anesthetics in 2016. Unsure if this will be true for many EDSers, but it’s an additional consideration. ALLOW FOR RARE PEOPLE TO EXIST.
And many of us are autistic or otherwise neurodivergent (ADHD and more) along with our families, so expect any and all manner of sensory processing disorders and variation, and sensitivity to lights, sounds, touch and more. We also have a lot of medical PTSD due to all of the above being so poorly known and recognized still.
END EMERGENCY CARE SECTION
Brief History and Description of EDS and the HSDs
The international Ehlers-Danlos Society (formerly the Ehlers-Danlos National Foundation or EDNF in the US until it was taken over by an English EDS patient with no medical training in 2016) or “TEDS” brought together some of the top minds in the field who drafted and produced the first major update to the nosology and diagnostic criteria for all forms of the Ehlers-Danlos syndromes since the Villefranche nosology was drafted in 1998.
Alas, it was biased toward thin white women with a Marfanoid Habitus like this cis-gendered leader, and toward enabling research for “the gene” yet to be found underlying hEDS, the only form without a SNP to pin it on yet. So the diagnostic criteria for hEDS were tightened a good bit, causing many to no longer be able to be diagnosed, or to even lose their diagnoses in some cases despite suffering plenty just the same.
This included describing a brand new diagnostic category called the Hypermobility Spectrum Disorders for all those who no longer met any EDS criteria (including the newly tightened hEDS criteria), but walked and talked like EDS patients just the same. (ICD-10 codes not established yet in 2023.)
Together with hEDS, these are intended to supplant and obsolete the old diagnoses of JHS, HMS and BJHS prior to 2017 per TEDS. People with these former diagnoses may retain them unless re-evaluated for some reason, and some areas and doctors are rejecting the new HSD diagnosis still as the 2017 diagnostic criteria have not been validated yet, just put forth by TEDS under Ms. Bloom.
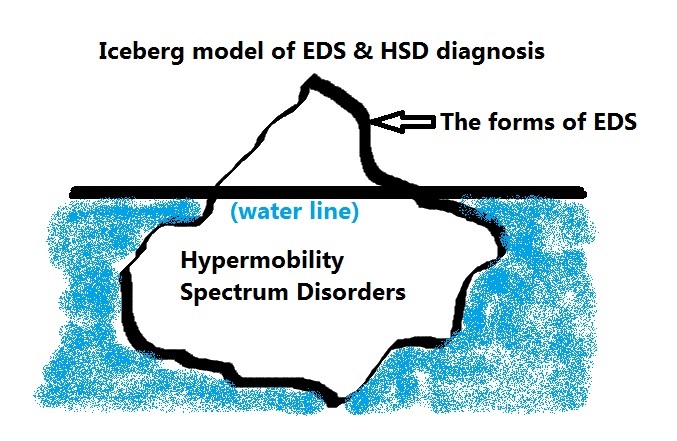
Think of these as the bulk of the iceberg below the water line, not medically visible to the diagnostic eye – until recently (2017).
These are patients who will have many signs of a systemic connective tissue disorder like EDS (including things like myopia, tendonitis, bursitis, subluxations, dislocations, stretchy skin, abdominal hernias, fallen arches, more), but do not fully meet the criteria for any of the currently 13 formally recognized forms of EDS, or similar Heritable Connective Tissue Diseases (HCTD) like Marfan syndrome, Stickler syndrome, Osteogenesis Imperfecta, or Loeys-Dietz syndrome.
But, like IBS and Fibromyalgia, (which happen to both be highly co-occurring in this population and probably results of having a CTD), the HSDs are currently still a diagnosis of exclusion.
NB PLEASE DO PROPER DIFFERENTIAL DIAGNOSIS, when diagnosing hEDS or an HSD, no matter how “easy” it seems to just diagnose either the most common hypermobile form of EDS (hEDS) or the new HSDs. It is very important to rule out all of the rare forms of EDS, as well as the similar appearing CTDS noted above. Here’s a little help differentiating Marfan Syndrom and/from Loeys-Dietz.
Diagnostic Flow Chart
| 1a – Do they seem like they have some kind of CTD? | 1b – Gather as much medical history as you can to see |
| 2a – Rule out all rare forms of EDS with genetic markers (12 of 13 as of 2024) | 2b – There are 12 types with markers per the 2017 nosology here |
| 3a – If negative by testing for those, then rule out all other possible similar CTDs like: | 3b – Marfans, Loeys-Dietz, Stickler Syndrome, Osteogenesis Imperfecta, Charcot-Marie Tooth |
| 4a – If negative for those, then rule out hEDS | 4b – No genetic test yet*, see hEDS Diagnostic Checklist |
| 5a – If negative for hEDS, then diagnose a form of Hypermobility Spectrum Disorder | 5b – This is a diagnosis of exclusion of ALL THE above! |
Be sure to rule out all rare forms of EDS, as well as:
- Marfan Syndrome
- Osteogenesis Imperfecta aka “Brittle bone disease” (bones break super easily)
- Stickler Syndrome
- Loeys-Dietz syndrome
- Charcot-Marie-Tooth Disease
- Weill-Marchesani Syndrome
- Pseudoxanthoma Elasticum
All doctors have seen EDS and HSD patients already whether you know it or not – we are the frequent flyers in your offices in fact, thanks to so many “issues with our tissues” without hitting your medical radar as having a systemic condition.
You just usually get us after we’ve aged prematurely and come down with arthritis, falling arches, weak teeth, thin skin, neuromas, detached retinas, etc. As some wise person once quipped (we don’t know exactly whom to credit yet):
“If you can’t connect the issues, think connective tissues.”
Anonymous, quoted by Dr. Heidi Collins in her 2014 talk of the same title, no longer available on YouTube
Be sure to Peel the Diagnostic Onion, and avoid falling short of a full and proper diagnosis. Especially if we are also autistic or have lots of allergies and sensitivities, autoimmune diseases or fibromyalgia. As a long time support group leader and observer of thousands in groups online, I’ve personally observed several major systemic conditions to run together quite often in hypermobile families, in what I have come to call the Chronic Constellation. Maybe one day we’ll know why.
Best Resources to Get Up to Speed Quickly
- EDS Toolkit for GPs (primary care doctors) now hosted by EDS UK (January 2022), originally hosted by the Royal College of General Practitioners in London since 2018 available to all to view. (I am one of the co-authors along with several of the world’s best specialists and doctors.)
- Temp down, 2023 TBD: Free online Physician EDS Education hosted by EDS Awareness since 2017 includes CMEs (John’s was one of the first sites to offer free CME’s about the new 2017 criteria)
- Project EDS ECHO hosted by The Ehlers-Danlos Society also offering CMEs for doctors (and additional ECHOs for other allied health professionals also since 2019).
- ER Safety Tips for Ehlers-Danlos Syndrome Patients – Ellen Lennox Smith 2017
- Ten Tips for Doctors by Jan Groh, author of this Oh TWIST site 2014
- All past EDNF and newer EDS Learning Conference slides 2012-present
ETA May 17, 2023: Check out these two new papers intended to guide medical practitioners in recognizing, diagnosing and treating hypermobile patients with chronic pain:
Hope for Hypermobility: Part 1—An Integrative Approach to Treating Symptomatic Joint Hypermobility
Hope for Hypermobility: Part 2—An Integrative Approach to Treating Symptomatic Joint Hypermobility
Daylor, Victoria BFA; Gensemer, Cortney PhD; Norris, Russell A. PhD; Bluestein, Linda MD
If this page has been helpful to you, would you please consider a donation of any amount, however small either one time or ongoing here, thank you. (I’m desperately poor due to disability still, and not being paid for all this medical education I’m providing for free, thanks.)
Additional Oh TWIST resources for those willing to read more in depth:
- When to Suspect HSD/hEDS / hypermobile Ehlers-Danlos syndrome
- When Else to Suspect HSD/hEDS etc.
- Why the hyper-focus on hypermobility may be misleading and ultimately harmful
- What are the new Hypermobility Spectrum Disorders
- Diagnosing HSD and EDS
- Common Comorbidities (there are even more than shown here)
- The Chronic Constellation most often seen in hypermobile and autistic families
- Additional Resources on the HSDs and EDS
- Recommended Books