Peeling the Diagnostic Onion
This isn’t going to be a post on how specifically to diagnose the Ehlers-Danlos syndromes (EDS) or Hypermobility Spectrum Disorders (HSD) per se, as that’s already been covered here.
Rather, I want to draw attention to the many “red herrings” or false leads that we and our doctors often identify and manage to recognize and diagnose much sooner and sometimes instead of a heritable connective tissue disorder you may really have underneath it all as well.
These comorbid diagnoses may not necessarily be wrong or inaccurate.
A la Hickam’s Dictum: patients are entitled to as many diseases as they damn please.
But, like red herrings, these comorbidities are often not the whole picture. They’ve led you down an exciting and productive diagnostic path, and once you hit the end of that particular path, you may incorrectly stop looking further. (Or your doctor may at least.)
The irony is, the Ehlers-Danlos syndromes usually come with one of the most visible clinical signs known: hypermobility of the joints. But they offer virtually no biomarkers (lab or other test results) for helping to diagnose them outside of genetic tests that won’t be ordered if they’re not suspected.
And the most common form by far, hypermobile EDS (hEDS) doesn’t even have a genetic marker to test for yet. So it is just a clinical diagnosis still.
So until and unless a doctor feels like they should suspect what they’ve been told is a really rare condition, they aren’t likely to order those genetic tests. Or even consider the clinical diagnosis of the even more common but hardly known yet Hypermobility Spectrum Disorders (invented in 2017).
But the autoimmune diseases do often have blood tests and biomarkers that can be checked. They will probably look for an elevated ANA, and check your C-reactive protein levels (CRP).If celiac disease is suspected they’ll look for some additional antibodies there. MS may exhibit some lesions on your nerves or brain. And RA and Lupus have their own markers too.
These are often the first and easiest things rheumatologists start to look for when patients come in complaining of diffuse and varying joint or body-wide or joint pain as we so often do with an HSD or EDS.
If these are negative, and nothing more obvious has clearly presented itself like Lyme Disease or a virus, you may get the super common “round file” diagnosis of Fibromyalgia, for lack of any better explanation of your diffuse and varying pain.
Toss in any GI issues and you’ll probably get diagnosed with the other catch-all bin called “IBS”, or Irritable Bowel Syndrome. Which may not be wrong, but just short-sighted too as I wrote here.
Those of you with diagnosed or suspected autism may also suspect and drill down to diagnose forms of mitochondrial disease or dysfunction, especially in your floppy babies or weak children who fatigue super easily.
Again, this may not be incorrect – many of the families I’ve met over the last six years had this going on too, properly diagnosed. But you may just be so very busy trying to manage these two things on top of any of your own medical issues (fibro, autoimmune disease), that you still don’t see or recognize the hypermobility in the family either, especially since no one has mentioned it to you.
And again, doctors will not have noticed it, as again, to date, they’ve been told that the Ehlers-Danlos syndromes are all quite rare, so will be rarely diagnosed. If you are still walking and talking, they probably won’t even consider it.
And to date (November 2018 as I write this), almost no doctors are even aware yet that the new subclinical category of the Hypermobility Spectrum Disorders was just newly recognized in March 2017 for all those with either milder signs of hypermobility but lots of issues with their tissues.
Or, if they are very bendy, who don’t seem to have much or enough trouble with their tissues to raise a flag for suspecting any Ehlers-Danlos syndrome – yet. (Yes, some can progress from a form of HSD to a full hypermobile EDS diagnosis over time. And vice versa.)
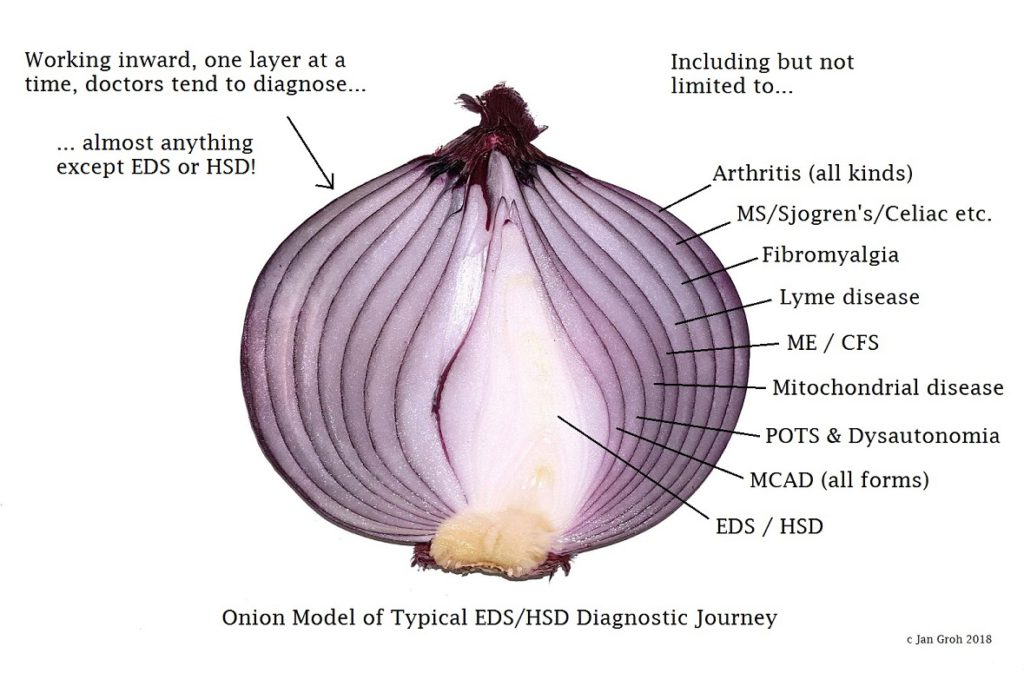
Image Description: Image made of a close up photo of a purple onion sliced in half against a bright white background, so that its layers are clearly showing. On the top left in black text it reads: “Working inward, one layer at a time, doctors tend to diagnose… (line break) … almost anything except EDS or HSD! “There is a thin arrow pointing from those words to the top left “shoulder” of the onion.
On the right hand side, all of the layers have been given suggested “diagnosis” labels (with thin lines tying them to the layers as you slowly go down the list, and inward in onion layers). Starting with: “Including but not limited to… Arthritis (all kinds), MS / Sjogren’s / Celiac etc. , Fibromyalgia, Lyme Disease, ME/CFS, Mitochondrial disease, POTS and Dysautonomia, MCAD (all forms), EDS/HSD “, (lastly, pointing to the center most white bit of onion). Copyright Jan Groh 2018.
For the most part, doctors have only been told about (or can only remember) the grossest signs of the rarest types of the heritable connective tissue disorders and word spreads extremely slowly if at all in medical circles, alas. (Unlike in patient circles.)
So you probably know more about all of this than 90% of doctors just now, no kidding! (This is why I’m pounding the keyboard so hard.) And they have to add it to the hundreds of other things they cram in their heads in medical school and residency.
Please be patient with them, as you bring them up to speed. They are very busy and smart people after all who aren’t just sitting around doing nothing. They are just not given much of a chance to learn about this subject in particular unless they knowingly seek it out as part of the Continuing Medical Education.
I liken it to how I did not keep up with the grade school math curriculum once I graduated 40 years ago right? Why would I, unless I happened to have kids who needed my help with theirs, and maybe not even then? Oh sure, I’ve kept on learning lots of things, just not the “New Math”, as it wasn’t required – for me.
And I would no more expect my GP or immunologist or psychologist to keep up with the latest in connective tissue disorders for the same reason: it doesn’t apply to them directly.
So again, if doctors don’t see gross signs of hypermobility and stretchy skin, they will probably stop considering anything physiological beyond fibromyalgia until and unless they learn about the new 2017 nosology and the Hypermobility Spectrum Disorders that were recognized then.
Nay, in fact, they may choose from any of this myriad of common comorbidities I’ve observed in the community. Which you may also have, but just in addition to a form of HSD or EDS or other heritable connective tissue disorder. Especially anxiety, depression, and sleep apnea.
Can you start to see how the forms of EDS and especially the new HSDs may get easily missed? We have a lot of possible onion layers to peel back before we may think to check for a hypermobility spectrum disorder or other connective tissue disorder. And a lot of missing or misinformation to overcome even when they are suspected.
I highly recommend the EDS Toolkit for General Practitioners I helped co-author with Dr. Reinhold this year (2018) to help get them up to speed the quickest. And other resources I have gathered for doctors on this page too.
Hypermobility Spectrum Disorders and CTDs are not rare… just rarely diagnosed! Last updated December 3, 2024.



Well written … totally relatable and tells an all too common story. I struggle to trust any GP or consultant but do my best to keep faith things will improve. All 3 of my children present with EDS related issues. I am diagnosed, they aren’t. The youngest was dxd with CRPS and IBS as well as severes disease. 3 NHS peds diagnosed. Sadly No one took it seriously and he suffered at school. I then home schooled. Social Services accused me of FI and I lost him to care system. This is happening too often…. a sad and drastic consequence happening to many innocent EDS parents.
I’m so sorry for your awful experience at the hands of medicine leading to this medical kidnapping of your son!! 🙁 Ack! This is why I’m writing. To hopefully quickly raise awareness of just how widespread this condition is in the population, and how widespread the issues can be and are in our bodies in those affected!!a
Stories like yours renew my determination to get my book out sooner than later. This has to come to light! Best wishes to you and your family. <3
More Drs need to know about this! My child who had other dx was medically kidnapped because they didn’t understand why he was so sick. Turns out he has Elhers Danlos, POTS, MALS, Gastroparesis along with a rare genetic bone dx. He was in state care for 6 months where terrible, unspeakable things happened. My child ended up being taken by ambulance to hospital 16x in those 6months because the state refused to believe he was sick. Drs need to be educated on this so this stops happening to innocent children & families!
I am so so sorry for your traumatic experience with your child being medically kidnapped and made to suffer so much from such lack of understanding!! This is why I write so much. To empower patients and doctors both to do better. Knowledge is power.
That said, please know that I’m also a co-author on the EDS Toolkit for Doctors here, hosted by the NHS at the moment: https://rcgp.org.uk/eds
And this is referenced all over the world. We just need more doctors to wake up and care. Few will study up on this particular area without a lot of prompting. (Any more than I would go back and learn the “New Math” since graduating highschool 40 years ago right? I don’t “have” to, so why would I? But if I was a doctor, well… maybe I should.)
Again, I’m so sorry for your experience! Hugs to you. x
This is such an important explanation of the experience of the diagnostic odyssey and what to expect. But more importantly, this is a fabulously clear resource for providers. Thank you for your advocacy work and bridging the gap!
Oh thank you so much for that! I’m glad it was so helpful. That is my intent and dearest wish. To shorten that diagnostic journey for everyone – patients AND doctors. Cheers.