EDS and IBS

One of the most common comorbidities of Ehlers-Danlos Syndrome (and, no surprise) Mast Cell Activation Diseases is IBS, or Irritable Bowel Syndrome.
Yes, we’re going to talk about our innards and toilet habits folks! This post is not for the squeamish. But then, life with EDS is not for the squeamish, and… this is a major part of our reality for a vast majority of us, if not all. And yes, you’ll wanna settle in again, it’s another longish read.
So what is IBS? For those unfamiliar, much like the term “Fibromyalgia”, “IBS” is another “catch-all” bin condition that is what you’re left with when you’ve eliminated all other possible causes of your GI distress and pain such as the flu, Crohn’s or colitis, or a parasite, or… etc.
In layman’s terms, it is a condition where you experience any and all forms of gut pain and discomfort and can experience wide variances in your bowel habits, from lots of constipation to sudden diarrhea – and sometimes both even in the same day. (And in one strange experience of my own recently: even at the same time – yes, truly – hold that thought.) As well as lots of gas and bloating.
Yes, you might want to put down any food you’re eating for the duration of this post! We’re gonna get real. Guess what? While unpleasant to talk about, everybody does poop – or surely should, and if they don’t, they’re in for some serious trouble if they’re not experiencing it already.
What goes in must (mostly) eventually come out, and in most cases (you folks with stomas excepted), it comes out the “other end”, or your bum, as the English say. (Those with ileostomies & colostomies please be patient with the rest of us.)
So pooping is a natural bodily function, and ideally should happen once a day, if not a couple times even. (Many folks find themselves ready and able to go in the morning after their first coffee or other stimulant of choice.) Yes, some people regularly poo two-three times a day depending on their diet and gut health (biome).
But some poo only 2-3 times per week. According to this source, anywhere from 2-3 times a day to 3 times per week is an acceptable range. (Beware of annoying pop up ads on this site, sorry, turn your speakers down.)
And if you’re healthy, you will form a semi-solid “log” daily (the proper term is “stool”) that lands right around a “4” on the Bristol Stool Chart. (Ideally, they say you should poop a “5” a couple times a day. I’ve only done this a couple of times in my life, but then the deck is stacked against me as you’ll see.)
Yes, there’s a poop chart, who knew! Now you can amuse your friends and torment your doctors (or is that torment your friends?) with your new-found insight into your poo. (I have bragged about my recently regular “4” to my doctor – he should be proud – it wasn’t easy to achieve with this lousy condition!)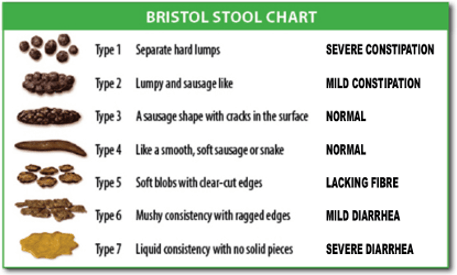
My naturopath told me our poo is made up of 50% bacteria in fact, so the healthier your gut biome (collection of intestinal bacteria we live with that helps us to digest food), the healthier (and better formed) your poo. (And usually easier to eliminate or emit.) And generally, a high natural (vegetable) fiber diet with plenty of water (not soda or dehydrating coffee) will help with this too.
But hold that thought. No surprise – where there is Ehlers-Danlos or hypermobility spectrum disorders, there are always exceptions! (If you’ve been reading my blog for any length of time you’ll be familiar with this drill by now. We put the “syn” in syndrome, and blow just about every curve you can find.)
Unsurprisingly, I was diagnosed with IBS early on in my diagnostic journey, not long after my appendectomy at age 20 in college. (I’ll never forget that, I tried to blame the dorm food – no dice.) The IBS pain I first experienced around age 23 started low and in the right quadrant, right around my appy scar. So we naturally looked for adhesions with ultrasound, but found none. This was in the early 1990’s too, mind you. (We knew a lot less than we do now back then.)
As I was a mildly stressed college-age female from a rough childhood in an alcoholic home, I was quickly written off as just “depressed with IBS”. Which wasn’t entirely inaccurate, but I now know many more of the drivers of both conditions, which I’ll now gladly share.
The medication given didn’t do much at all for me, so I ended up giving it up (probably wise in 20/20 hindsight). This was also true for the SSRI’s I tried through the years – in fact, one (Wellbutrin) made me mildly psychotic once. Yet, because doctors have SSRI hammers, everything is an SSRI nail.
(Please do NOT stop taking your SSRI’s or other medications because of anything I say, and do so only in a very slow step-wise fashion under medical supervision with your doctor’s approval – there can be major side-effects of doing so. I never stayed on them long, so never had a problem stopping. And they can and DO help some people, just not all, or even a majority as some are finding. And there are MANY drivers of depression in us as I wrote about here.)
Yet the pain never subsided, and in fact, slowly grew to encompass my entire lower innards, from the duodenum on down. (I now hurt from my stomach on down, constantly.) I suffered wildly varying bowel habits, with regular bouts of constipation punctuated by sudden bouts of diarrhea with lots of bloating and gas on top, and rarely the occasional “balanced” day or two in a row.
I ate a very “Standard American Diet” at the time, including lots of bread and other carbs (pastas, cakes, cookies), even though I probably ate more fresh and cooked veggies and less actual candy and sweets than many. (I was brought up on a very mid-western style/German home-cooked meat and potatoes diet with some veggies on the side and not much junk thankfully. Eating out was a treat.) I did also drink a little alcohol – not a lot, thanks to my childhood experience. (I no longer drink at all – it’s a trigger now.)
Needless to say I learned early on about adding fiber to battle the constipation but ironically found doing so swung my system wildly to the other direction – and too much so. I loved gardening and included plenty of my own fresh veggies and tossed in a decent amount of fruit though I found it hard to digest. But nothing seemed to break this mad GI cycle, and I suffered mostly silently through my young adulthood with no true relief.
At one point I had both upper and lower GI studies done, only finding I had a mildly slow transit time, but nothing further. (No ulcers, diverticuli, or worse, knock wood.)
I slowly learned to navigate my diet and found a combo of carbs, meat and veggies that helped me achieve a slightly more “normal” elimination schedule and experience. But I never got any good answers to this problem and stopped consulting doctors who unfailingly prescribed…. yup, SSRI’s. (If only I could have seen a naturopath 20 years ago!)
Fast forward to early 2012, and my sudden EDS onset “storm” or “cascade” that took me from walking to wheelchair in just 3 weeks at almost 45 years old. And suddenly I began to find some answers to all my issues – including, no surprise, my IBS.
Not only did I find it to be extremely commonly comorbid in the EDS support groups I was in (on and offline), but also in the comorbid MCAD support groups I ended up in also.
I also got to consult a naturopath (finally) in latter 2012 who recommended both finding all my food sensitivities via the Basic e95 food panel (blood test), and taking a rather expensive but comprehensive therapeutic level probiotic she highly recommended as the only one that gave consistently good results in her experience.
Needless to say my blood panel came back showing I was reactive to all the foods I had been eating the most – especially eggs and gluten and beef. But also tomatoes, dairy, yeast, and more. So much for my fried eggy sandwiches! (I’ve since done an IgE test and it was negative, so all of these are IgG driven obviously, knock wood. I’d have been much more anaphylactoid otherwise I’m sure. I mostly just exhibit high histamine levels, some call “histamine intolerance”.)
My ND admitted it might be hard, but urged me to try my best to go on a full elimination diet after the holidays in January 2013. That is, eliminating all the foods we found me moderately or more sensitive to. I was interrupted in this plan by the need to visit my poorly aunty (a Catholic nun) back east when she suddenly entered hospice in a coma in February 2013 and I flew back to be with her for two weeks. She rallied and I just saw her again for her 70th Jubilee (at almost 92) but needless to say, I had to eat whatever I was offered as the guest of the convent, so all dietary bets were off.
However, I’d landed in a great holistic EDS support group online in the meantime, where I was exposed to all kinds of great functional and holistic medical info, including an introduction to leaky gut and the much touted GAPS (Gut and Psychology Syndrome) Diet for fixing it there. (There are other diets that can help, and you should work with your chosen practitioner – whether ND or MD to find the right one for you.)
Upon looking up leaky gut, I realized this made a lot of sense in light of not only our weak epithelial layers, but all of our likely comorbid gut dysbiosis, comorbid SIBO and proclivity to gluten sensitivity. Which some say gives everyone leaky gut whether they know it or not.
I quickly realized the GAPS Diet would “kill two birds with one stone” so to speak for me: start to help heal my gut, and definitely eliminate all my food sensitivities! So I started it in earnest upon returning.
The GAPS diet takes you down to just a bone broth of choice to start (during the “Intro” phase), then you slowly add only whole foods back in just one at a time, only one every 3 days so you can truly detect any reactions and sensitivities. The collagen filled bone broth helps soothe your poorly gut and help it start to heal. Absolutely no hard fibers or roughage allowed for several weeks so the poor thing can start to truly heal.
Lo and behold – I found my pain reduced, gut calmer, sleep improved, brain fog improved, memory improved, and so much more. Not least of which was elimination improved also. Who knew what all inflammation could do until you eliminated it. (Well okay, all you smart functional medicine types out there, I know I know. Bear with us while the rest of us catch up!)
I then took a webinar on leaky gut and Small Intestinal Bacterial Overgrowth (aka SIBO, pronounced “see-boe”) and learned that you can have a stuck ileo-cecal valve between your large and small intestines that can allow gut bugs to back up into your small intestine lending to this overgrowth.
They proceeded to describe how you can actually manually massage your ileo-cecal valve closed if it’s open, but I haven’t had the nerve (er, guts? sorry) to try this myself. But it struck me that this is likely true in folks with EDS – who have weak valves and connective tissues all over. I’m betting we are the so called “tough cases” these guys talk about so much.
This excess of bugs there then also lends to leaky gut as the little buggers produce something called (I’m not making this up!) “zonulin” (so Trekkie sounding, lol!) which helps loosen your tight-gap junctions in your gut, causing “leaky” gut allowing over-sized food molecules to pass through.
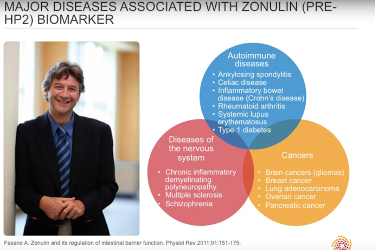
So instead of perceiving it as a friendly food protein, it’s seen as an invading substance and your immune system is triggered to activate and “attack” it. Whence all the inflammation, which can help drive autoimmune diseases too. Poor innocent lentil!
Did I mention that sugar encourages all the wrong/bad bugs to thrive, who produce the most zonulin? Of course they do. Cuz, EDS.
Toss in low stomach acid on the top end failing to kill enough bugs on the way down, and voila: SIBO which causes loads of excess gas, bloating and discomfort. And lots of belching, farting, etc. Ding! I had all the signs of this also, no surprise.
Good news, you can get better with either natural herbal remedies, or in worst cases a course or two of anti-biotics to clear up the excess. Which you then want to quickly repopulate via health pro-biotics before any “bad guys” can get a foothold and produce more zonulin. Going low/no-sugar including natural sugar can really help too.
That said, I’ve not been surprised to find this a recurring problem (nay, even intractable) among EDS patients, as I’m betting our weak connective tissue lends to a chronically leaky ileo-cecal valve constantly allowing for this back up.
And I’m trying to remember what Dr. Meglathery told me may be causing the chronically low stomach acid (possibly a thyroid imbalance if my presently leaky memory serves? I need to look this up again – hypothyroidism is rampant among us too, no surprise), but it came up while discussing her RCCX and Illness Theory this past spring (2016). I think I caught a comment recently that CRH or cortisol may lower stomach acid. Still looking for backup on this.
And don’t let experiencing GERD fool you either – it doesn’t mean you have sufficient stomach acid either. I’ve also learned that your esophageal sphincter won’t fully close until it senses enough acid in your stomach – and the stomach produces acid in response to histamine (whence H2 blockers being prescribed for lots of MCAD patients, aka Zantac, Pepcid).
So no wonder so many experience GERD with EDS and MCAD of any kind, despite actually having naturally low stomach acid at baseline. Thankfully mine cleared up as soon as I stopped drinking coffee years ago – apparently a trigger for me. I don’t miss it, frankly.
Toss in common hiatal hernias and weak sphincters all over and no wonder we’re sort of doomed digestively speaking. But wait, there’s more! (Of course there is cuz… EDS!)
Then, I learned that diarrhea and GI upset (nausea, etc.) are all common signs of MCAD reactions and low level anaphylaxis, and I began noticing and tracking many more reactions than before. Bye bye coconut, sigh.
But, between eliminating most of my triggers, upping my anti-histamines and adding quercetin (a natural mast cell stabilizer), lowering my stress, eating more organic whole foods (almost exclusively now), adding a therapeutic probiotic (more on that in a minute) and avoiding sugar, and voila: my healthy “4” on the Bristol Stool chart. Usually. 😉
Now, having said that, I got a wild hair one day this last year to eat a bunch of steamed fresh broccoli after I’d had a rare bout of constipation from a medication I took. No, not an opioid either, though those are a common problem for us. Gee, what could possible go wrong?
Uhm, well, the broccoli could turn out to be a trigger (I hadn’t had any in a long time, and not in that quantity), and I ended up experiencing something I later termed “diapation” (alternatively: constarrhea?). This was where I had the strongest urge to eliminate ever, just like I was about to have explosive diarrhea, and yet, not a blessed thing came out!! Nothing! Not even a tiny little rabbit poop. Nada. Sigh.
Oh my word, talk about anguish. The old bathroom stall rhyme came to mind:
“Here I sit, broken-hearted, tried to sh*t but only farted” (author unknown, see bathroom stall walls worldwide). Whoever crafted that is genius. And probably had IBS. And MCAD.
Normally when I have constipation, I don’t also have such a strong elimination urge. I just feel… full. Yes, I want to poop, but I can manage to function albeit unpleasantly at a semi-normal level for a day or two. What surprised me about the broccoli was the absolute certainty I had that I was about to explode with terrible diarrhea, and yet… nada. Truly like a combo of both diarrhea (the urge) and constipation. (Inability to move.) Weirdest experience ever!
Someone in one of my MCAD support groups suggested this was my large bowel dry spasming from my reaction to the broccoli. I believe it, as I felt the broccoli go all the way through my system in a complete spasm, like a rock. All. The. Way. Through. Yes, painful. Take an esophageal spasm, one of my other deep joys through the years, and extend it through the entire digestive tract, following the food bolus as it goes down.
Thankfully, I clearly at least have decent motility – that is, ability to push food through my system and out the other end eventually. Some poor folks with EDS are plagued with another complication called Gastroparesis: literally stomach paralysis. This causes your food to simply sit and rot in your stomach or small bowel, making you quite sick. Basically it’s like constipation but much higher up the system. (Aka dysmotility.)
They suffer terribly from malnutrition and malabsorption as the food never gets properly moved through the system in a timely fashion. Some poor folks end up on feeding tubes and formula just to stay alive. I’m so very grateful that’s not me! I only experience some mild early satiety and anorexia (lack of appetite, not nervosa) in general. Both worsened a lot when I started to react to chlorine in water from swimming and tap water in late 2015. I did lose twenty pounds then and grew quite weak until I could eat again after discovering this cause.
Needless to say, food sitting and fermenting in your upper GI tract will also lend to increased gas and bloating (and inflammation). So those poor folks have yet another driver to that fun. Some of this is driven by MCAD, but even more by neuropathic trouble likely from an impinged vagus nerve.
I’ve come to recognize sudden my bouts of gastric pain (gastritis) and bloating followed by either constipation or diarrhea to be typical with my MCAS reactions now. (MCAD is the umbrella term for all forms, including MCAS and mastocytosis, NB.)
And of course, as too many of you know too well, opioids induce constipation big time. Thankfully I only suffered a couple months at my worst, as I quickly found mild strengthening as soon as I started Vitamin C, so I could wean off my pain killers. I now only need one on occasion, at most 3x/week generally only if I bust a move. but no more constipation from that thankfully.
I did not take any regular pain meds besides OTC Tylenol and Ibuprofen before 2012. I now live at an average of 5 overall on the pain scale and am fine as long as I can stay there. I have some hot spots that like to spike higher pretty quickly, but I can handle it most of the time, whence only the occasional use now vs daily at my worst in 2012.
No, no fun. Yes, it’s been quite a journey. I’m so grateful I ate my way through France back in 2001 when I was relatively mildly afflicted. Not unafflicted, just less so. So when my doctor ordered me to “please eat!” earlier this year during my chlorine reaction (until I figured that out), I nearly smacked him – he should know I’m a foodie! (I love food, it just doesn’t all love me.)
 Happily, I’ve returned to my new peri-menopausal “normal” since eliminating chlorine and fluoride from my life this year. (I’m also back up to a healthy 115 lbs at 5’4″.) And oh yeah, did I mention that hormone changes can make all of this worse for women? Yeah. Toss that on the steaming heap of drivers of our gastric pain and discomfort. Estrogen is a mast cell trigger, progesterone makes you more lax, whee. Girls don’t wanna have that much fun, but alas we get it! And they call us wimps…
Happily, I’ve returned to my new peri-menopausal “normal” since eliminating chlorine and fluoride from my life this year. (I’m also back up to a healthy 115 lbs at 5’4″.) And oh yeah, did I mention that hormone changes can make all of this worse for women? Yeah. Toss that on the steaming heap of drivers of our gastric pain and discomfort. Estrogen is a mast cell trigger, progesterone makes you more lax, whee. Girls don’t wanna have that much fun, but alas we get it! And they call us wimps…
Protip: if you gradually lose your appetite altogether -aka anorexia (not nervosa) – and struggle to get almost anything down for a period of time, it’s probably something you’re eating/drinking/are in touch with daily like chlorine in your water, or fluoride in your toothpaste and/or water. (You can get a cheap 5 stage filter from ZeroWater from many larger department stores to help eliminate both if you live in an apartment on SSD like me.)
And oh yeah, MCAD can cause sudden onset of nausea and vomiting at any time. I knew I forgot something! I’ve just had mine so well controlled for so long I’d forgotten – lucky me. But so can twisting wrong (often to the left) and suddenly impinging your vagus nerve. So many causes… so little time! Remember to solve for both x and y with this lousy condition – always!
I warned you it would be quite a journey didn’t I? Hopefully not too much for you! To those who love us and are trying to support us, thank you or being there with us through thick and thin – literally. To those of you suffering with all of this along side me, and who take every meal you keep down as a success, high five and hang in there, and keep those probiotics coming.
It’s not an easy fix, but like all of our issues, I find a multi-faceted approach to work best. Mine consists of a combo of detoxing, stress, sugar and trigger elimination (both food and chemical), an organic whole food diet that works for me (mostly GF DF and grain-free high nat sat fat paleo diet except for oatmeal now), a really good probiotic (I now take just L. Rhamnosus as Culturelle on the Cusack Protocol), lots of steamed veggies that I tolerate, some kale juice on occasion, and my daily Reiki.
Oh, and lots of water, salt and potassium along with all my supps (C, D3, calc, mag, zinc and more) so it all “sticks”. You need magnesium and potassium and salt to actually re-hydrate fully. Plain water tends to go right through us – see the RCCX Theory for likely reasons why pertaining to the CYP21A2 gene.
I still have chronic constant gut pain, but again, my bowel habits are much more regular and ‘smooth’ compared to before. I can live with this much better than the alternative and will, TYVM. All drug-free. (That is, no drugs taken specifically for “IBS”.)
I hope this helps some of you sort out some of your issues too, EDS or no. (And remember, those of you with “Fibromyalgia” are probably hypermobile too IMHO.)
Wow, I’ve actually worked up an appetite writing this. I’m gonna go eat my rations for dinner and call it a night. At least I got something done while all the fireworks were going on – outside this time. 😉
Happy US Fourth of July,
Jandroid 3.141592658

Thank-you so much for this article: I have come to the conclusion that I have EDS-H, after a random article suggestion a month or two back while I was researching something else entirely! I have been experiencing joint pains with frequent subluxations since I was 17 (I am now 40), and started experiencing gastric issues in my later 20’s. when I was 30 I was diagnosed with Crohn’s disease after I got peritonitis from a ruptured lesion in my small intestine (which was initially thought to be a ruptured appendix, but wasn’t). Then, because I also had joint symptoms, I was diagnosed with Crohn’s associated arthritis and fibromyalgia, and put on a delightful triple therapy of methotrexate, azapress and a quinolone, which only made me worse. The only thing which helped the pain was opiates and cortisone. After a few years (during which I ditched my gastroenterologist and rheumatologist and had a genetic screening which picked up a couple of connective tissue issues), I had cause to see a different gastroenterologist, who performed another colonoscopy and a gastroscopy, and who put me on meds for reflux, and referred me to a different rheumatologist, telling me that this doctor would probably put me on DMARDs. However, the new rheumatologist said he thought that I actually had joint hypermobility syndrome with repetitive strain injury (ironically he here chose to quote the story of the hooves, horses and zebras!), and told me to avoid endurance sport and get a job in academia (I am a physiotherapist, and had already had to give up my practice due to intractable joint pain). This made much more sense to me, but I was offered no further input or advice, and was just told to manage the symptoms. Now I am of the opinion that I have never had Crohn’s disease, and that all my different health problems are actually caused by EDS!
Ah bless you, so glad you found my site, and better yet, found it so helpful! I always say “trust – and heal – your gut!” – literally! I too was written off as just depressed with IBS years ago, so I stopped complaining and just managed my diet myself as best I could, finding the careful combo that kept my innards happier than not.
Thing is, women often eventually get worse – and diagnosed – during peri-menopause due to our hormone changes, even if not measurable. (Dr. Meglathery thinks we may respond to a percursor of the measurable form of progesterone, so it goes undetected while we suffer in her RCCX Theory here: http://rccxandillness.com . I’m betting she’s right.)
Anyway, I strongly suspect any/all with Fibro and any additional GI issues and/or sensitivities (especially “Multiple Chemical Sensitivity”) – this is identical to MCAD symptoms and mild EDS I see, TYVM. But… nope, we only see horses as you said. (Funny they did quote that, right?)
Anyway, glad you found me, and I could help validate some of your feelings. Use my resources pages to ‘gird your loins” and inform your doctors with the latest and greatest info. Good luck, and welcome to the giant “Clan Dumpty” where all the King’s Horses (should be zebras, smile) and all the King’s Men can’t put us back together again – or not as easily as they’d like. 😉
http://ohtwist.com/eds-resources/
http://ohtwist.com/what-is-mcad/mcad-resources/
Thank-you so much for your prompt, encouraging and informative response! I have read the link you sent to Dr. Meglathery’s website: it sounds like there will soon be several breakthroughs in understanding all these conditions (though whether these will translate to treatment options remains unclear).
NB someone just sent me an email saying that they found the ZeroWater filter mentioned above does NOT eliminate fluoride. I did not know this as I’m lucky: I live in Portland, OR where we voted down fluoride in our city water! (Thank heavens, and thanks everyone who did, please continue!) So once I eliminated fluoride in my toothpaste, I was fine again. And it DOES filter out chlorine (or I wouldn’t be fine, I promise.)
I’m bummed, as I could swear they advertised that they did, but… just keep this in mind and seek a better, possibly reverse-osmosis filter in that case.
Just been diagnosed with fibromyalgia and hypermobility at the age of 17. So confused as to whether I have EDS or just hypermobility. My rhem says I have benign hypermobility. I am going to a naturalist soon so I’m excited to get some relief. Does the diet and the things you mentioned help with joint pain as well? I’m so depressed to be going through this and being so young.
So sorry to hear that, but… the younger you suspect it, the better off you’ll be as you can start eating right sooner than I did. And yes, eating right can/does help all of the related issues to some degree.
Very few rheumatologists believe in or will diagnose any form of EDS yet, even hte most common one, HEDS, as they’ve only been told about the grossest signs of the rarest types. Scour my site for guidance to arm yourself with good info to help further suspect. Also try to get as much family medical history as you can to help them suspect it in your family.
The posts may help the most:
http://ohtwist.com/2015/05/24/when-else-to-suspect-ehlers-danlos-syndrome/
http://ohtwist.com/about-eds/diagnosing-eds/
http://ohtwist.com/2014/05/20/but-im-a-horse/
And my resources pages here:
http://ohtwist.com/eds-resources/
http://ohtwist.com/eds-resources/finding-support/
http://ohtwist.com/eds-resources/recommended-books/
I hope that helps. Stay strong, always believe in yourself, trust -and heal – your gut. I’d try to find a naturopath or functional medicine doctor to help you along, diagnosed or not. And try to find a support group on or off line so you can find some kindred spirits to share the journey with.
Good luck, Jan
What about chlorine encountered via skin contact (no chlorine/fluoride in our local tap water that I am aware of)? I do water-ex 4-5 times per week at a local pool when at home. Have had chronic diarrhea for the past 15 years. When I don’t do it, or am on vacation, I have normal stools. I don’t intentionally swallow pool water, but wondered if skin contact is enough to cause this sort of GI reaction. I’d hate to give it up, but I think malabsorption is possibly causing my hair to thin drastically. Thoughts?
Yes, actually, you can totally absorb chlorine through your skin as well as by ingesting it in your tap water. This is how I got so sick 3 years ago and ended up dropping so much weight when I couldn’t eat. It was a combo of all of the above: drinking unfiltered chlorinated tap water, using fluoride toothpaste (plus getting a filling impregnated with fluoride), and swimming about twice a week in chlorine. Too much!
The next most mind-blowing thing I’ve learned? >Scents< can give you diarrhea too! That's my new latest problem: people's perfume and marijuana smoke and some cooking odors have been giving me GI distress. I never thoguht that could be true, but it is. As soon as I get away from the odors - all is well! And there's lots of chlorine odor (gas) around swimming pools too. Don't stop swimming though... just be mindful, maybe cut back a touch or try to find a saline pool if you can... (I've got one, but just can't afford it right now, waah). HTH!
I get diapation relatively frequently, personally – any time my gut swings too rapidly from constipation to diarrhea. Fairly simple mechanical process in my case; constipation past a certain point usually leaves a little bit behind after elimination, but the diarrhea following it – due to its softness – requires a much greater pressure to push this “plug” out than more constipation would.
Oh interesting! Glad to know someone else experiences that weird combo besides me! I was just surprised to be constipated by broccoli of all things…
Oh my goodness, this nearly has me in tears. We expect hEDS in our family, but we’ve been struggling to get diagnosed (a lot of insurance denials). I also suspect MCAS and POTS. We’ve been searching for a diagnosis for two years now because of symptoms my kids have shown. I’ve always had wobbly, loose joints but I started with POTS symptoms after my first pregnancy (seven years ago) and my gastro symptoms started two years ago (literally on the night of my 31st birthday). I usually can manage, but I’m in one of my worst flares of everything and it’s just so frustrating to feel like doctors will look for everything except what I ask them to. (Between family members, we check off high percentages of symptoms for hEDS, POTS, MCAS, fibromyalgia, etc.)
Long story short, thank you for posting this. Reading through this and reading an experience that follows so closely to mine at least makes me feel less alone and crazy.
(I also am in Oregon – just south of Portland.)
Ahh you’re welcome Mel, and welcome – to the great Clan Dumpty, of Humpty fame, right? They can’t seem to put us back together again, if they even see that we’re cracked open. And welcome, Portland neighbor! If you’re not already, I highly recommend joining the Official Oregon Area EDS support group on Facebook here:
https://www.facebook.com/groups/341049939429534/
I also have an OhTWIST support group on Facebook. but if you prefer to avoid the book – I’m also on MeWe here now:
https://mewe.com/join/ohtwist
Anyway, trust – and heal – your gut. You definitely have plenty of signs of a Hypermobility Spectrum Disorder of some kind, if not outright EDS or related, yes. And, you’re definitely not alone!